Table of Contents
Introduction: The Unique Calling of Oncology Nursing
Embarking on a career in nursing is a significant undertaking, demanding intellect, compassion, and resilience. Choosing to specialize within this vast field adds another layer of dedication. Among the most challenging and profoundly rewarding specializations is oncology nursing. This field focuses on the comprehensive care of patients diagnosed with cancer, spanning the entire continuum from prevention and screening through diagnosis, treatment, survivorship, and end-of-life care. Oncology nursing requires a unique blend of advanced clinical skills, deep scientific knowledge, exceptional communication abilities, and profound empathy.
For nursing students considering or currently navigating this specialty, the path can seem daunting. The complexities of cancer biology, the intensity of treatments, the emotional weight carried by patients and families, and the ever-evolving nature of the field demand rigorous preparation and unwavering commitment. However, the impact an oncology nursing professional can have on a patient’s life during their most vulnerable moments is immeasurable. It’s a specialty that offers incredible opportunities for professional growth, intellectual stimulation, and deep personal satisfaction.
This article is as a comprehensive guide for students, outlining the key knowledge domains in oncology nursing and providing practical strategies for academic and clinical success, ultimately preparing them for a fulfilling career in this vital area of healthcare. The journey into oncology nursing is demanding, but with the right knowledge and approach, students can thrive and become invaluable members of the cancer care team.
I. Understanding the Landscape: Core Knowledge Areas in Oncology Nursing
Success in oncology nursing begins with a robust understanding of its fundamental principles. Students must build a strong theoretical foundation upon which practical skills can be layered. This involves delving into the science of cancer, treatment modalities, symptom management, and the psychosocial dimensions of care.
A. The Science of Cancer: Foundational Principles
At its core, oncology nursing is grounded in the science of cancer. Students need a solid grasp of:
- Cancer Biology and Pathophysiology: Understanding how normal cells transform into malignant ones is crucial. This includes knowledge of the cell cycle, gene mutations (oncogenes, tumor suppressor genes), angiogenesis, invasion, and metastasis. Familiarity with the hallmarks of cancer provides a framework for understanding treatment targets.
- Common Cancer Types: While it’s impossible to be an expert in every cancer, students should develop knowledge of the epidemiology, risk factors, clinical presentation, diagnostic workup, and general treatment approaches for prevalent cancers (e.g., breast, lung, colorectal, prostate, hematologic malignancies).
- Staging and Grading: Understanding cancer staging systems (like TNM) and tumor grading is essential for comprehending prognosis, treatment planning, and patient communication. This knowledge helps the oncology nursing professional interpret reports and anticipate patient needs.
B. Pillars of Treatment: Navigating Therapeutic Modalities
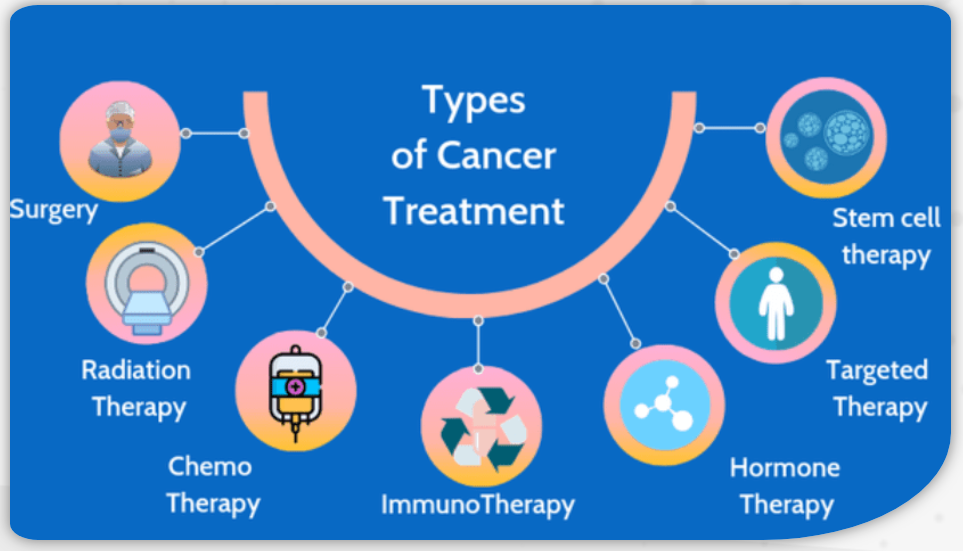
Oncology nursing professionals are intimately involved in the administration and management of various cancer treatments. Students must learn the principles, procedures, potential side effects, and specific nursing considerations for each:
- Surgical Oncology: Understanding pre-operative preparation, intra-operative support (though often specialized), and post-operative care is vital. This includes wound management, pain control, monitoring for complications (e.g., infection, bleeding, lymphedema), and patient education regarding recovery.
- Chemotherapy and Biotherapy: This is often a central component of oncology nursing. Key areas include:
- Principles of cytotoxic agents, targeted therapies, and immunotherapies.
- Safe handling and administration protocols (including personal protective equipment).
- Vascular access device management (ports, central lines).
- Recognition and management of acute and chronic side effects (e.g., myelosuppression, nausea/vomiting, mucositis, neuropathy, cardiotoxicity, infusion reactions).
- Patient education regarding self-care during treatment.
- Radiation Therapy: Nurses working with radiation oncology patients need to understand:
- Different types of radiation (external beam, brachytherapy).
- Principles of radiation safety (time, distance, shielding).
- Management of radiation-specific side effects (e.g., skin reactions, fatigue, site-specific toxicities like mucositis or enteritis).
- Psychosocial support for patients undergoing daily treatments.
- Immunotherapy and Targeted Therapies: These newer modalities represent a significant shift in cancer care. Oncology nursing requires knowledge of:
- Mechanisms of action (e.g., checkpoint inhibitors, CAR T-cell therapy, monoclonal antibodies).
- Unique side effect profiles (e.g., immune-related adverse events – irAEs) which can affect any organ system and require prompt recognition and management.
- Specific administration and monitoring requirements.
- Hematopoietic Stem Cell Transplantation (HSCT): This intensive therapy requires specialized oncology nursing knowledge, including:
- Conditioning regimens and their toxicities.
- Infection prevention during profound immunosuppression.
- Management of Graft-versus-Host Disease (GVHD).
- Long-term follow-up care.
- Hormonal Therapy: Understanding its use in hormone-sensitive cancers (e.g., breast, prostate), mechanisms of action, and management of side effects (e.g., hot flashes, bone density loss).
C. Managing the Journey: Symptom Control and Palliative Care
A cornerstone of excellent oncology nursing practice is effective symptom management. Cancer and its treatments often cause distressing symptoms that significantly impact quality of life. Students must become proficient in assessing and managing:
- Pain: Comprehensive pain assessment (using validated scales), understanding different types of cancer pain (nociceptive, neuropathic), principles of pharmacologic management (opioids, adjuvants), non-pharmacologic interventions, and addressing barriers to effective pain control.
- Nausea and Vomiting: Assessment of chemotherapy-induced nausea and vomiting (CINV), understanding antiemetic classifications and schedules, non-pharmacologic strategies, and managing anticipatory or delayed CINV.
- Fatigue: Recognizing cancer-related fatigue (CRF) as distinct from normal tiredness, assessment strategies, and evidence-based interventions (e.g., exercise, energy conservation, addressing contributing factors like anemia or depression).
- Nutritional Deficits: Screening for malnutrition, managing anorexia and cachexia, addressing taste changes, providing nutritional counseling, and understanding indications for enteral or parenteral nutrition.
- Other Common Symptoms: Managing mucositis/stomatitis, diarrhea, constipation, skin toxicities, dyspnea, anxiety, depression, sleep disturbances, and cognitive changes (“chemo brain”).
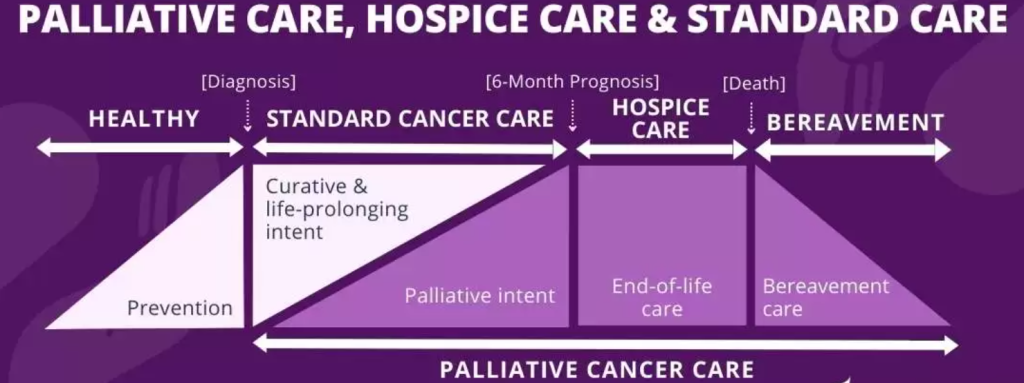
- Integrating Palliative Care: Understanding that palliative care focuses on improving quality of life through symptom management and psychosocial support, and should be integrated early in the cancer trajectory, not just at the end of life. Oncology nursing plays a key role in advocating for and providing palliative interventions.
D. The Human Element: Psychosocial Support and Communication
Cancer impacts not just the body, but the entire person and their family system. Effective oncology nursing necessitates strong psychosocial skills:
- Therapeutic Communication: Actively listening, demonstrating empathy, using open-ended questions, providing clear and honest information, and validating patient and family emotions. Mastering difficult conversations (e.g., discussing prognosis, treatment failure, end-of-life preferences) is crucial.
- Psychosocial Assessment: Screening for distress, anxiety, depression, coping mechanisms, social support systems, and spiritual needs.
- Supporting Coping: Helping patients and families navigate the emotional rollercoaster of diagnosis, treatment decisions, side effects, recurrence fears, and survivorship challenges.
- Ethical Dilemmas: Recognizing and navigating complex ethical situations common in oncology nursing, such as informed consent, treatment futility, resource allocation, and patient autonomy, particularly near the end of life.
- Cultural Competence: Understanding how cultural beliefs and values influence health decisions, communication styles, family involvement, and perceptions of illness and death. Providing culturally sensitive care is paramount.
E. Empowering Patients: Education and Advocacy
Oncology nursing professionals are key educators and advocates. Students must learn to:
- Provide Effective Patient Education: Tailoring complex information about diagnosis, treatment plans, potential side effects, self-care measures, and follow-up schedules in a way patients and families can understand and retain. Using teach-back methods is essential.
- Help Navigate Health Information: Assisting patients in finding reliable sources of information and discerning credible data from misinformation, especially online.
- Act as Patient Advocates: Ensuring patients’ wishes are heard and respected, helping them navigate the complex healthcare system, coordinating care among different specialists, and advocating for access to necessary resources and support services.
F. Beyond Treatment: Survivorship and End-of-Life Care
The scope of oncology nursing extends beyond active treatment:
- Survivorship Care: Understanding the potential long-term physical and psychosocial effects of cancer and its treatment, developing survivorship care plans, promoting healthy lifestyle behaviors, screening for late effects and secondary malignancies, and addressing issues like fertility, employment, and insurance.
- End-of-Life Care: Providing compassionate, holistic care focused on comfort and dignity for patients nearing the end of life. This involves expert symptom management, facilitating communication about goals of care, supporting family members through the grieving process, and collaborating with hospice teams. This aspect of oncology nursing demands immense sensitivity and skill.
II. Strategies for Success: Thriving as an Oncology Nursing Student
Mastering the vast knowledge base of oncology nursing is only part of the equation. Students also need effective strategies to navigate their coursework, clinical experiences, and the emotional demands of the specialty.
A. Mastering Academics: Building a Strong Foundation
The academic component of oncology nursing education can be intense. Success requires proactive learning and effective study habits:
- Active Learning: Don’t just passively read. Use techniques like concept mapping, creating flashcards for medications and side effects, forming study groups, and teaching concepts to peers.
- Resource Utilization: Fully leverage textbooks, reputable journals (e.g., Clinical Journal of Oncology Nursing, Oncology Nursing Forum), online resources from organizations like the Oncology Nursing Society (ONS), and institutional library databases.
- Time Management: Break down large amounts of information into manageable chunks. Create a study schedule and stick to it, balancing coursework with clinical rotations and personal life.
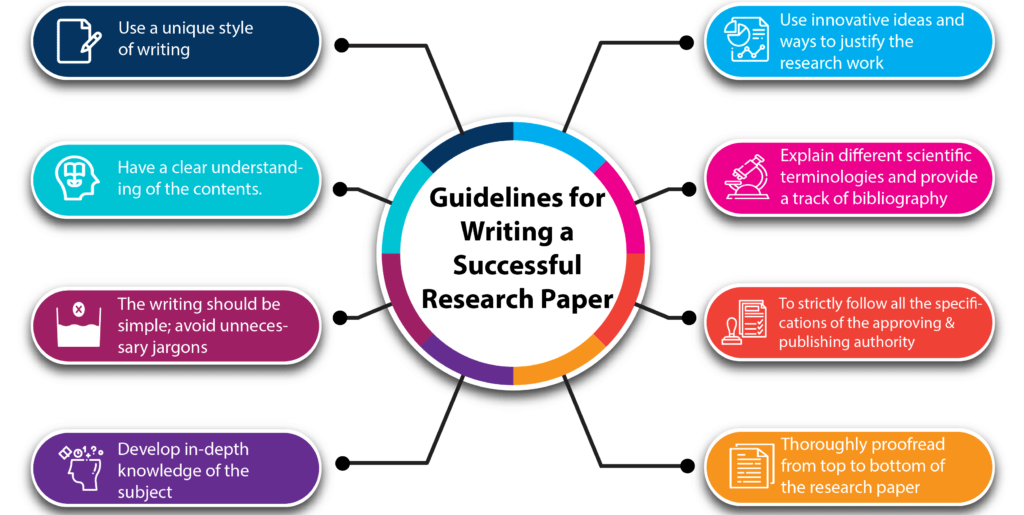
- Tackling Assignments: Academic assignments are designed to deepen understanding and critical thinking.
- An oncology nursing essay might require you to explore an ethical dilemma, discuss the nurse’s role in a specific treatment modality, or analyze the impact of a particular symptom. Focus on a clear thesis, strong evidence, and logical argumentation.
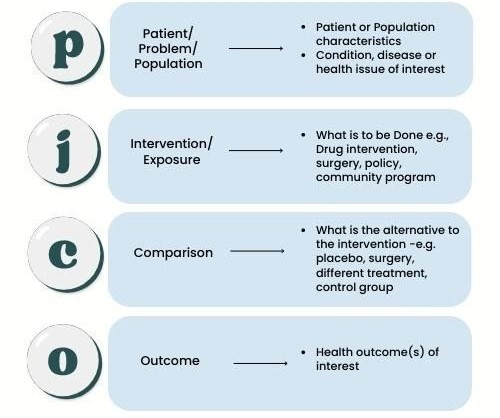
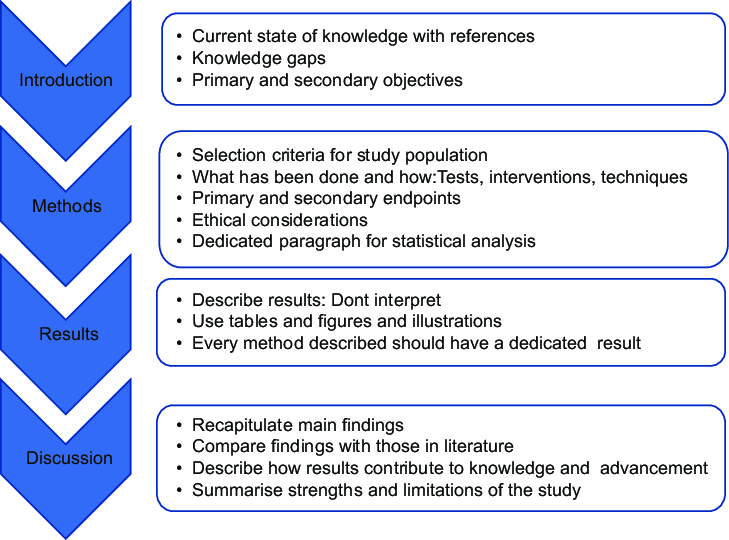
- An oncology nursing research paper demands more in-depth investigation. This could involve a literature review on a specific intervention’s effectiveness or exploring trends in survivorship care. Rigorous research methods, proper citation, and critical analysis are key.
- Any oncology nursing assignment, whether a presentation, care plan, or short paper, should demonstrate your grasp of core concepts and your ability to apply them. Pay close attention to the instructions and grading rubric.
- Developing a compelling oncology nursing case study is an excellent way to integrate theory and practice. Select a complex patient scenario (real or hypothetical, respecting confidentiality), detail the assessment, nursing diagnoses, interventions, evaluation, and relevant pathophysiology and psychosocial considerations. This showcases holistic oncology nursing skills.
Need help with writing authentic an impactful oncology nursing essay, research paper, case study, dissertation or TEAS exam? PhD Nurse Writer has experienced and dedicated writers to help you with oncology nursing topic suggestion, paper writing, proofreading, editing, formatting and plagiarism removal.
B. Excelling in Clinical Practice: Translating Knowledge into Action
Clinical rotations are where theoretical knowledge comes to life. Maximize these experiences:
- Preparation is Key: Before each clinical day, review your patients’ diagnoses, treatment plans, medications, and potential complications. Formulate learning objectives.
- Develop Assessment Skills: Hone your ability to perform thorough physical assessments, focusing on systems commonly affected by cancer and treatments. Learn to recognize subtle changes that could indicate complications. Practice psychosocial assessment and symptom assessment using validated tools.
- Master Technical Skills: Seek opportunities to safely practice skills like administering chemotherapy (under supervision), managing central lines, performing wound care, and operating infusion pumps. Always prioritize safety protocols.
- Communicate Effectively: Practice therapeutic communication with patients and families. Observe experienced oncology nursing professionals interacting with patients. Participate actively in interdisciplinary rounds and handoffs.
- Seek Feedback: Ask questions of your preceptor, clinical instructor, and staff nurses. Be open to constructive criticism and use it to improve your practice. Reflect on your experiences daily.
- Embrace Interprofessional Collaboration: Understand the roles of physicians, pharmacists, social workers, dietitians, chaplains, and other team members. Effective oncology nursing relies heavily on teamwork.
C. Cultivating Resilience: Caring for Yourself While Caring for Others
Oncology nursing is emotionally demanding. Witnessing suffering, dealing with loss, and managing complex care situations can lead to stress, compassion fatigue, and burnout. Proactive self-care is not a luxury; it’s a necessity:
- Recognize the Signs: Be aware of the symptoms of burnout and compassion fatigue (e.g., emotional exhaustion, cynicism, reduced sense of accomplishment, physical symptoms).
- Implement Self-Care Strategies: Prioritize sleep, nutrition, and exercise. Engage in hobbies and activities outside of nursing. Practice mindfulness, meditation, or journaling.
- Debrief and Seek Support: Talk about challenging experiences with trusted colleagues, mentors, or supervisors. Utilize employee assistance programs or counseling services if needed. Participate in unit debriefing sessions after critical events.
- Set Boundaries: Learn to balance empathy with professional boundaries. It’s important to care deeply, but also to protect your own emotional well-being.
- Celebrate Small Victories: Acknowledge the positive impact you make, even in small ways. Find meaning and purpose in your work.
D. Building Connections: Networking and Mentorship
Connecting with others in the field can provide invaluable support, guidance, and career opportunities:
- Join Professional Organizations: Become a student member of the Oncology Nursing Society (ONS) or your local chapter. Access educational resources, journals, networking events, and scholarship opportunities.
- Find Mentors: Seek out experienced oncology nursing professionals—faculty members, clinical preceptors, or staff nurses—who can offer guidance, share insights, and support your professional development.
- Attend Conferences and Workshops: Participate in educational events (even virtual ones) to learn about the latest advancements, network with peers and experts, and gain inspiration. The field of oncology nursing is dynamic, and these events help you stay current.
E. Embracing Lifelong Learning: The Evolving Field of Oncology Nursing
Cancer care is constantly evolving with new research, treatments, and technologies. A commitment to lifelong learning is essential for any oncology nursing professional:
- Stay Current: Regularly read professional journals, attend webinars and in-services, and follow reputable oncology news sources.
- Pursue Certification: Once eligible, consider pursuing specialty certification, such as the Oncology Certified Nurse (OCN®) credential offered by the Oncology Nursing Certification Corporation (ONCC). Certification demonstrates specialized knowledge and commitment to excellence in oncology nursing.
- Consider Advanced Education: Explore opportunities for graduate education (Master’s or Doctoral degrees) to become an advanced practice nurse (Nurse Practitioner or Clinical Nurse Specialist), educator, researcher, or administrator in oncology nursing.
III. The Future of Oncology Nursing: Trends and Opportunities
The field of oncology nursing is dynamic, shaped by scientific breakthroughs and evolving healthcare models. Students entering the field should be aware of key trends:
- Precision Medicine and Genomics: Treatments are becoming increasingly tailored based on the genetic makeup of a patient’s tumor. Oncology nursing will involve educating patients about genomic testing, interpreting results, and managing targeted therapies.
- Immunotherapy Expansion: As immunotherapies become more common and used in various combinations, nurses will need continued education on managing complex immune-related adverse events.
- Telehealth and Remote Monitoring: Technology is playing a larger role in symptom monitoring, patient education, and follow-up care, requiring new skills in virtual oncology nursing.
- Focus on Health Equity: Addressing disparities in cancer incidence, access to care, and outcomes among different populations is a growing priority. Oncology nursing professionals are crucial advocates for equitable care.
- Expanding Role of Advanced Practice Nurses (APRNs): Oncology NPs and CNSs are taking on increasingly complex roles in managing patient care, leading clinics, and conducting research.
- Growth in Ambulatory and Community Oncology: More cancer care is shifting to outpatient settings, requiring oncology nursing expertise in managing complex treatments and providing education outside the traditional hospital environment.

Conclusion: Embracing the Challenge and Reward of Oncology Nursing
Choosing a path in oncology nursing is a commitment to a specialty that demands continuous learning, clinical excellence, and profound compassion. It involves navigating the scientific complexities of cancer, mastering intricate treatment regimens, skillfully managing distressing symptoms, and providing unwavering psychosocial support to patients and families during life-altering journeys. The academic challenges, including crafting a thoughtful oncology nursing essay or a detailed oncology nursing case study, are stepping stones to developing the critical thinking required in practice.
For students drawn to this field, the journey requires dedication, resilience, and a strong support system. By building a solid knowledge base, honing clinical skills, prioritizing self-care, seeking mentorship, and embracing lifelong learning, aspiring oncology nursing professionals can not only succeed but thrive.
The challenges are significant, but the rewards—the privilege of making a tangible difference in the lives of those affected by cancer, the intellectual stimulation of a constantly evolving field, and the deep human connection forged through compassionate care—are unparalleled. Oncology nursing is more than a job; it is a calling for those dedicated to providing expert, holistic care when it matters most. The future of cancer care relies on the next generation of skilled, knowledgeable, and compassionate oncology nursing leaders.