Table of Contents
Medication errors are a pervasive issue in healthcare, with potentially devastating consequences for patients. To understand the intricacies of these errors and find ways to mitigate them, healthcare professionals rely on rigorous analysis. One powerful tool for this analysis is the medication error case study.
A well-written medication error case study goes beyond simply describing the error. It delves into the underlying factors, analyzes the consequences, and proposes solutions. This article serves as a comprehensive guide, providing clear guidelines for crafting a stellar medication error case study that informs, educates, and inspires action.
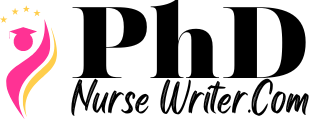
What is Medication Error in Nursing?
Medication error in nursing refers to any preventable event that may cause or lead to inappropriate medication use or patient harm while under the care of a nurse. This can occur at any stage of the medication process, from prescribing and dispensing to administration and monitoring.
Here are some common examples of medication errors in nursing:
- Wrong medication: Administering the wrong drug or a drug with a similar name.
- Wrong dosage: Giving a dose that is too high or too low.
- Wrong route: Administering medication through the wrong route (e.g., giving an oral medication intravenously).
- Wrong time: Administering medication at the wrong time, such as giving a medication that should be given before meals after a meal.
- Wrong patient: Giving medication to the wrong patient.
- Missed dose: Failing to administer a scheduled dose of medication.
- Incorrect preparation: Failing to properly prepare or reconstitute a medication before administration.
- Lack of monitoring: Failing to monitor the patient’s response to medication or to recognize adverse effects.
- Poor communication: Miscommunication between healthcare providers about medication orders or patient allergies.
Factors contributing to medication errors in nursing:
- Work overload and stress: Nurses often work long hours under pressure, increasing the risk of errors.
- Poor communication: Miscommunication between nurses and other healthcare professionals can lead to errors.
- Lack of training and education: Nurses may not be adequately trained in medication administration or may lack knowledge about specific medications.
- Systemic factors: Poorly designed medication systems, inadequate staffing levels, and lack of resources can contribute to errors.
- Patient factors: Patient factors, such as age, language barriers, or cognitive impairment, can make medication administration more challenging.
Consequences of medication errors:
- Patient harm: Medication errors can lead to a wide range of adverse effects, including allergic reactions, organ damage, and death.
- Increased healthcare costs: Medication errors can result in prolonged hospital stays, readmissions, and costly legal settlements.
- Erosion of trust: Medication errors can damage the patient’s trust in the healthcare system.
Preventing medication errors:
- Improved communication: Implementing clear communication channels between nurses and other healthcare professionals.
- Enhanced training and education: Providing nurses with comprehensive training on medication administration and patient safety.
- Use of technology: Employing electronic medication administration systems and bar coding to reduce the risk of errors.
- Promoting a culture of safety: Creating an environment where nurses feel comfortable reporting errors and near misses.
- Standardization of medication practices: Developing and implementing standardized procedures for medication administration.
- Medication reconciliation: Performing medication reconciliation at each transition of care to ensure accurate medication lists.
- Patient education: Educating patients about their medications, potential side effects, and the importance of reporting any concerns.
Medication errors are a serious issue in healthcare. By understanding the contributing factors, consequences, and prevention strategies, nurses can play a crucial role in improving patient safety and reducing the incidence of these preventable events.
How to Write a Stellar Medication Error Case Study
1. Defining the Scope: Identifying the Right Case
Not every medication error case study is created equal. Before embarking on the writing process, it’s crucial to identify a case that offers the potential for insightful analysis and valuable learning.
- Relevance and Impact: Choose a case with significant implications for patient safety, ideally one that led to adverse events or near misses. This ensures the study’s impact and relevance to the broader healthcare community.
- Novelty and Insights: Look for cases that present unique perspectives or address emerging challenges in medication safety. This ensures the study’s contribution to the existing body of knowledge.
- Ethical Considerations: Ensure the case study respects patient privacy and confidentiality. Obtain informed consent from the patient or their legal representative, if applicable.
2. Gathering and Analyzing Data: Building a Strong Foundation
Once you’ve chosen a case, the next step is to gather comprehensive data to support your analysis. This includes:
- Patient Information: Gather relevant patient information, including demographics, medical history, and allergies, ensuring privacy and confidentiality are maintained.
- Medication Information: Detail the medication involved, including its purpose, dosage, route of administration, and any relevant warnings or precautions.
- Timeline of Events: Reconstruct the sequence of events leading up to the error, including who was involved, what actions were taken, and what communications occurred.
- Error Analysis: Identify the specific error that occurred, classify it using established frameworks like the National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) system, and analyze its root cause.
- Consequences: Document the consequences of the error, including immediate and long-term effects on the patient’s health and well-being.
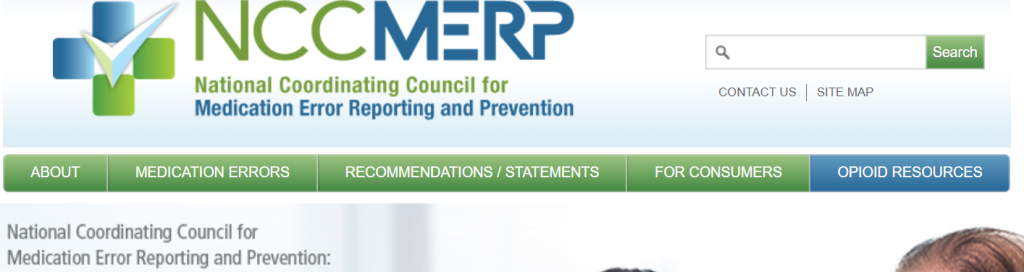
3. Structure and Content: Guiding the Reader Through the Study
The structure of your medication error case study should be clear and logical, guiding the reader through the analysis. A typical format includes:
- Introduction: Briefly introduce the case, highlighting its relevance and significance. State the purpose of the study and outline the key questions it aims to address.
- Case Description: Provide a detailed description of the medication error, including the patient, the medication involved, the specific error, and the circumstances surrounding the event.
- Analysis: This section forms the core of the case study. Analyze the factors contributing to the error, using a framework like the Swiss Cheese Model or the Human Factors Analysis and Classification System (HFACS).
- Discussion: Discuss the findings of your analysis, highlighting the significance of the error and the implications for patient safety.
- Recommendations: Based on your analysis, propose specific recommendations for preventing similar errors in the future. These recommendations should be practical, actionable, and evidence-based.
- Conclusion: Summarize the key takeaways from the case study, emphasizing the importance of medication safety and the need for ongoing efforts to improve patient care.
4. Writing Style: Engaging and Informative
The writing style of your medication error case study is crucial for effectively communicating your findings.
- Clear and Concise Language: Use clear, concise language, avoiding jargon and technical terms unless they are essential.
- Objectivity and Impartiality: Maintain objectivity throughout the case study, presenting the facts without bias or personal opinions.
- Engaging Narrative: While maintaining objectivity, strive for an engaging narrative that captures the reader’s attention. Use vivid language and specific examples to illustrate your points.
- Logical Flow: Organize your thoughts and ideas in a logical and coherent manner, using headings, subheadings, and transitions to guide the reader through the study.
- Visual Aids: Use tables, graphs, and diagrams to present data in a clear and visually appealing manner.
5. Ethical Considerations: Protecting Patient Privacy and Confidentiality
When writing a medication error case study, ethical considerations are paramount.
- Informed Consent: Obtain informed consent from the patient or their legal representative before using their information in the case study. This ensures they are aware of the study’s purpose, potential risks, and benefits.
- Confidentiality: Protect patient privacy by de-identifying all patient information, using pseudonyms or altering identifying details. Ensure that no information can be used to identify the individual.
- Sensitivity and Respect: Treat the patient with respect and sensitivity throughout the study. Avoid using language that could be considered stigmatizing or disrespectful.
6. The Power of Collaboration: Working with a Team
Writing a stellar medication error case study often requires collaboration with others.
- Multidisciplinary Team: Include professionals from different disciplines, such as nurses, pharmacists, physicians, and patient safety specialists. This ensures a comprehensive perspective and a more robust analysis.
- Patient Involvement: If possible, involve the patient in the case study. Their perspective can provide valuable insights and contribute to the study’s impact.
- Feedback and Review: Seek feedback from colleagues, mentors, and experts in medication safety. Their insights can help strengthen the study’s content and quality.
7. Dissemination and Impact: Sharing Your Findings
The ultimate goal of a medication error case study is to make a positive impact on patient safety.
- Target Audience: Identify your target audience, considering their level of knowledge and interests. This will help you tailor your writing style and content for maximum impact.
- Publication Options: Consider publishing your case study in peer-reviewed journals, professional newsletters, or online platforms. This ensures wider dissemination and reach.
- Presentation and Discussion: Present your case study at conferences, meetings, or educational events. This provides an opportunity to engage with colleagues and discuss the findings.
Examples of Engaging Medication Error Case Studies
Here are examples of compelling topics for a medication error case study.
- Medication Error Case Study: Incorrect Dosage Administration – This could explore a scenario where a patient received an incorrect dosage of medication due to a miscalculation, transcription error, or lack of proper drug knowledge.
- Medication Error Case Study: Wrong Drug Administration – This could focus on a situation where a patient received the wrong medication entirely, perhaps due to similar-sounding names or a confusing medication order.
- Medication Error Case Study: Allergic Reaction Due to Lack of Allergy Information – This case study could analyze a situation where a patient experienced a severe allergic reaction after receiving a medication they were unaware they were allergic to, highlighting the importance of thorough allergy documentation.
- Medication Error Case Study: Drug Interaction Overlooked – This could explore a scenario where a patient experienced adverse effects due to an overlooked drug interaction, demonstrating the necessity of comprehensive drug interaction checks.
- Medication Error Case Study: Lack of Patient Education – This could examine a situation where a patient failed to adhere to medication instructions due to inadequate education or communication regarding their medication, emphasizing the crucial role of patient education.
- Medication Error Case Study: Lack of Standardized Protocols – This could analyze a situation where a medication error occurred due to inconsistent procedures or the absence of standardized protocols for medication administration, highlighting the importance of clearly defined workflows.
- Medication Error Case Study: System-Wide Error Analysis – This could examine a larger-scale incident involving multiple medication errors, focusing on identifying the root causes, contributing factors, and system-wide solutions to prevent future occurrences.
Remember, each of these medication error case study topics offers opportunities to investigate specific contributing factors, analyze the impact on patient safety, and develop strategies for improvement.
9. The Importance of Continuous Improvement:
Medication errors are complex and multifaceted, and there is no single solution to eliminate them entirely. However, by leveraging the power of a medication error case study, we can learn from past mistakes, identify vulnerabilities in our systems, and implement interventions to prevent future errors.
Common Pitfalls in Case Study Writing and How to Avoid Them
Writing a medication error case study can be a valuable tool for learning and improving patient safety. However, several pitfalls can compromise the effectiveness of the study. Here’s how to avoid them:
1. Lack of Clear Objectives:
- Pitfall: The study lacks a clear purpose, leading to a rambling narrative with no clear conclusions.
- Solution: Define specific objectives for the medication error case study. What lessons do you want to learn? What changes are you hoping to implement? Clearly stating your objectives will guide your writing and analysis.
2. Over-simplification of the Error:
- Pitfall: The study focuses on a single factor, ignoring the complex interplay of factors that contributed to the error.
- Solution: Conduct a thorough root cause analysis. Identify all contributing factors, including human error, system failures, and environmental factors. This comprehensive approach will provide a more accurate understanding of the medication error case study and lead to more effective solutions.
3. Lack of Patient Perspective:
- Pitfall: The study focuses solely on the medical side, neglecting the impact of the error on the patient.
- Solution: Include the patient’s perspective on the error. How did it affect their physical and emotional well-being? Their experience can provide valuable insights for improving patient safety.
4. Insufficient Data and Documentation:
- Pitfall: The medication error case study lacks sufficient data to support its conclusions.
- Solution: Gather comprehensive data and documentation. This includes patient medical records, medication administration records, incident reports, and relevant policies and procedures. Robust data will strengthen the credibility of your medication error case study.
5. Ignoring Systemic Issues:
- Pitfall: The study blames individuals for the error without addressing underlying system vulnerabilities.
- Solution: Focus on identifying and addressing system-level issues that contributed to the error. This could include inadequate training, unclear communication protocols, or poor workflow design. Improving the system will prevent similar errors from happening in the future.
6. Lack of Actionable Recommendations:
- Pitfall: The medication error case study ends without concrete recommendations for improvement.
- Solution: Develop specific and measurable recommendations for preventing future errors. These recommendations should be based on the findings of the study and address identified systemic issues.
7. Lack of Confidentiality:
- Pitfall: The study divulges confidential patient information, violating privacy regulations.
- Solution: Ensure strict confidentiality throughout the medication error case study. Use de-identified data and avoid disclosing any personally identifiable information about the patient.
By avoiding these pitfalls, you can create a medication error case study that is informative, insightful, and impactful, ultimately leading to improved patient safety.
Frequently Asked Questions about Medication Error Case Studies
- What is the purpose of a medication error case study? A medication error case study serves several purposes. It can help to:
- Identify the contributing factors to the error.
- Analyze the impact of the error on the patient.
- Develop strategies to prevent similar errors in the future.
- Improve patient safety by promoting awareness and understanding of medication error risks.
- What are the essential elements of a good medication error case study? A strong medication error case study should include:
- A clear description of the error and its context.
- The patient’s perspective and any potential impact on their health.
- Analysis of the contributing factors, including human error, system failures, or communication breakdowns.
- Recommendations for improvement and how to mitigate future risks.
- How can I find real-life examples of medication error case studies? You can find medication error case studies in various sources:
- Professional journals and publications: Look for publications related to healthcare quality, patient safety, and medication administration.
- Healthcare organizations and agencies: Organizations like the Joint Commission and the Institute for Healthcare Improvement often publish case studies.
- Online databases: Search for case studies using relevant keywords and phrases.
- What ethical considerations should be addressed in a medication error case study? Maintaining patient confidentiality and anonymity is crucial. The study should be conducted in a way that respects the patient’s privacy and protects sensitive information. Additionally, the study should avoid identifying individuals involved, using fictionalized names and details if necessary.
- How can I use a medication error case study to improve medication safety in my own setting? By reviewing and analyzing medication error case studies, you can gain valuable insights into potential risks and weaknesses in your own practices. You can use this knowledge to:
- Develop and implement stronger medication safety protocols.
- Improve communication and collaboration among healthcare professionals.
- Enhance patient education and understanding of their medications.
- Strengthen your organization’s commitment to continuous improvement and patient safety.
The Bottom Line: Building a Culture of Safety
Following these guidelines will enable a healthcare professional to craft a compelling medication error case study that illuminates the complexities of medication safety and inspire positive change. These studies serve as valuable resources for:
- Improving Patient Care: By analyzing past errors, we can learn to prevent future mistakes and ensure safer medication practices.
- Educating Healthcare Professionals: Case studies provide real-world examples that enhance learning and promote a culture of safety.
- Advocating for Change: Through the dissemination of findings, we can raise awareness, influence policy, and advocate for improved systems and processes to enhance medication safety.
A medication error case study plays a vital role in building a culture of safety in healthcare. By embracing these guidelines, we can harness the power of these studies to improve patient care and create a healthcare system that is safer for everyone.
Get Help with Writing a Medication Error Case Study
Writing a stellar medication error case study can be a daunting task for most students. But, why go through all the stress when you can simply order an original paper from PhD Nurse Writer? We can deliver an authentic medication error case study, tailored to your specific needs and goals. Our nursing paper writing help covers research papers, essays, case studies and dissertations.