
Table of Contents
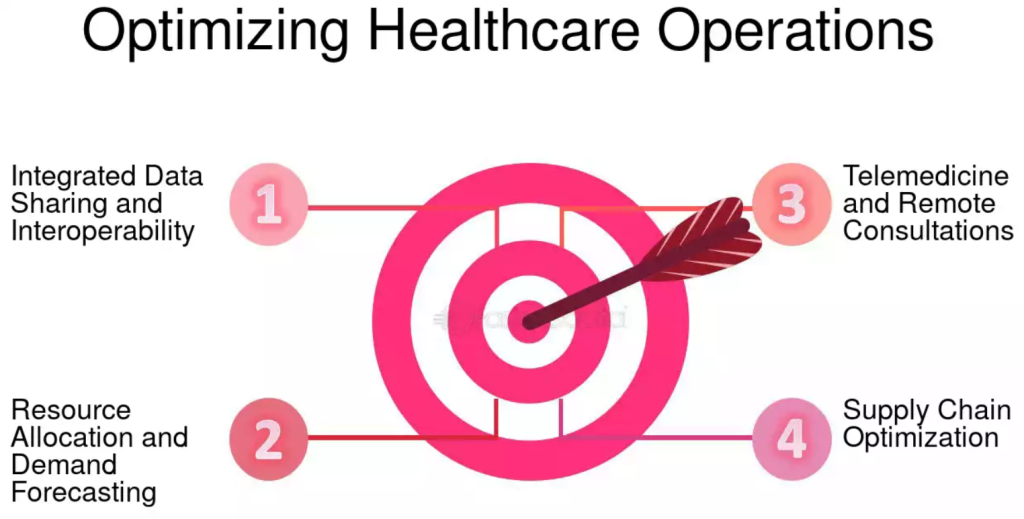
Healthcare systems worldwide stand at a critical juncture. Faced with aging populations, rising chronic disease burdens, escalating costs, workforce shortages, and the rapid pace of technological advancement, the need for transformation is undeniable. The status quo is no longer sustainable, nor does it consistently deliver the high-quality, equitable, and patient-centered care that individuals deserve. The solution lies in a continuous, multi-faceted process: optimizing healthcare.
This comprehensive guide delves into the core principles, strategies, challenges, and future directions involved in this essential undertaking. Optimizing healthcare isn’t a single initiative but a persistent commitment to improving every facet of care delivery, from the individual patient encounter to the systemic policies that shape the health landscape.
The concept of optimizing healthcare encompasses enhancing clinical outcomes, improving patient experiences, increasing operational efficiency, reducing costs, supporting the well-being of the healthcare workforce, and leveraging technology and data to drive better decisions. It requires a holistic view, recognizing that these elements are interconnected and interdependent. True progress in optimizing healthcare demands collaboration among clinicians, administrators, policymakers, researchers, technology developers, patients, and communities.
Why is Optimizing Healthcare Imperative?
The urgency for optimizing healthcare stems from several converging pressures:
- Unsustainable Costs: Healthcare expenditures consume a significant and growing portion of GDP in many nations, straining government budgets, businesses, and individuals.
- Variable Quality: Despite high spending, care quality and patient outcomes can vary dramatically depending on location, provider, and socioeconomic status.
- Patient Expectations: Patients are increasingly informed and demand more personalized, convenient, and transparent care experiences.
- Workforce Burnout: Clinicians and healthcare staff face immense pressure, leading to burnout, turnover, and potential impacts on patient safety.
- Technological Potential: Advances in digital health, AI, and data analytics offer unprecedented opportunities for improvement, yet adoption and integration lag.
- Health Equity: Significant disparities in access and outcomes persist across different populations, highlighting systemic failures that need addressing.
Addressing these challenges head-on through deliberate strategies for optimizing healthcare is not just desirable; it’s essential for the health and well-being of populations and the sustainability of the systems designed to serve them.
Pillar 1: Enhancing the Patient Experience and Access
At its heart, healthcare is about people. Therefore, a primary focus of optimizing healthcare must be on the patient. This involves moving beyond a purely clinical perspective to embrace patient-centered care, where individuals are active partners in their health journey.
Key Strategies:
- Improving Access to Care:
- Expanding telehealth services for remote consultations, monitoring, and follow-ups.
- Optimizing scheduling systems to reduce wait times.
- Addressing geographical barriers through mobile clinics or community health worker programs.
- Simplifying insurance processes and promoting price transparency.
- Ensuring culturally competent care that respects diverse backgrounds and needs.
- Enhancing Communication and Engagement:
- Implementing patient portals for secure messaging, access to records, and appointment scheduling.
- Utilizing shared decision-making tools to involve patients in treatment choices.
- Providing clear, understandable health information and education materials.
- Actively soliciting and responding to patient feedback through surveys and advisory councils.
- Creating Seamless Care Journeys:
- Improving care coordination between primary care, specialists, hospitals, and post-acute care settings.
- Developing personalized care plans that address the patient’s holistic needs, including social determinants of health.
- Ensuring smooth transitions of care to prevent readmissions and errors.
Focusing on the patient experience is fundamental to optimizing healthcare, as satisfied and engaged patients are more likely to adhere to treatment plans and achieve better health outcomes.
Pillar 2: Advancing Clinical Quality and Patient Safety
Optimizing healthcare inherently means delivering the safest, most effective care possible, grounded in evidence and focused on continuous improvement. This involves minimizing errors, adhering to best practices, and rigorously measuring outcomes.
Key Strategies:
- Promoting Evidence-Based Medicine:
- Ensuring clinicians have access to and utilize the latest clinical guidelines and research findings.
- Integrating clinical decision support tools within Electronic Health Records (EHRs).
- Encouraging participation in clinical trials and research.
- Strengthening Patient Safety Protocols:
- Implementing robust systems for error reporting and analysis (e.g., root cause analysis).
- Utilizing checklists and standardized procedures for high-risk processes (e.g., surgery, medication administration).
- Investing in technologies that reduce specific risks, such as barcode medication administration.
- Fostering a culture of safety where staff feel empowered to speak up about concerns without fear of retribution.
- Measuring and Reporting Outcomes:
- Defining and tracking key quality indicators (KQIs) across various conditions and procedures.
- Using patient-reported outcome measures (PROMs) to capture the patient’s perspective on their health status.
- Benchmarking performance against peers and national standards.
- Using data analytics to identify areas for improvement and track the impact of interventions.
A relentless focus on quality and safety is non-negotiable in the quest for optimizing healthcare. Every prevented error and improved outcome represents a significant step forward.
Pillar 3: Driving Operational Efficiency and Cost-Effectiveness
Waste in healthcare – whether through inefficient processes, unnecessary tests, or administrative complexity – diverts resources from patient care. Optimizing healthcare requires streamlining operations and ensuring financial sustainability.
Key Strategies:
- Process Improvement Methodologies:
- Applying Lean principles to identify and eliminate waste in workflows (e.g., patient flow, lab turnaround times, documentation).
- Using Six Sigma methodologies to reduce variation and defects in processes.
- Mapping value streams to understand and improve the sequence of activities that create value for the patient.
- Resource Management:
- Optimizing staff scheduling and deployment based on patient demand.
- Improving supply chain management to reduce inventory costs and prevent stockouts of essential items.
- Implementing energy efficiency programs and sustainable practices.
- Utilizing predictive analytics for better capacity planning and resource allocation.
- Reducing Administrative Burden:
- Streamlining documentation requirements through EHR optimization and voice recognition tools.
- Automating routine administrative tasks (e.g., billing, coding, prior authorizations) where possible.
- Simplifying referral processes and inter-departmental communication.
- Value-Based Purchasing and Payment Models:
- Shifting from fee-for-service models (which incentivize volume) to models that reward value (quality outcomes relative to cost).
- Participating in Accountable Care Organizations (ACOs) or bundled payment initiatives.
Operational efficiency is a critical enabler for optimizing healthcare, freeing up resources and time to be reinvested in direct patient care and quality initiatives. Effective cost management ensures the long-term viability of healthcare services.
Pillar 4: Supporting the Healthcare Workforce
The individuals delivering care are the most valuable asset in any healthcare system. Burnout, dissatisfaction, and turnover directly impact patient care quality, safety, and experience. Therefore, optimizing healthcare must include strategies to support the well-being and engagement of the workforce.
Key Strategies:
- Addressing Burnout and Promoting Well-being:
- Implementing programs focused on mental health support, stress management, and resilience training.
- Optimizing workloads and schedules to promote work-life balance.
- Reducing administrative burdens that contribute to frustration (as mentioned in Pillar 3).
- Creating supportive and respectful work environments.
- Investing in Training and Development:
- Providing ongoing education and professional development opportunities.
- Training staff on new technologies, procedures, and communication skills (e.g., empathy, shared decision-making).
- Developing clear career pathways and leadership opportunities.
- Fostering Engagement and Teamwork:
- Encouraging interprofessional collaboration and communication.
- Empowering staff to participate in decision-making and quality improvement initiatives.
- Recognizing and rewarding contributions and excellence.
- Creating a culture of psychological safety and mutual respect.

A supported, engaged, and resilient workforce is fundamental to successfully optimizing healthcare delivery at the front lines.
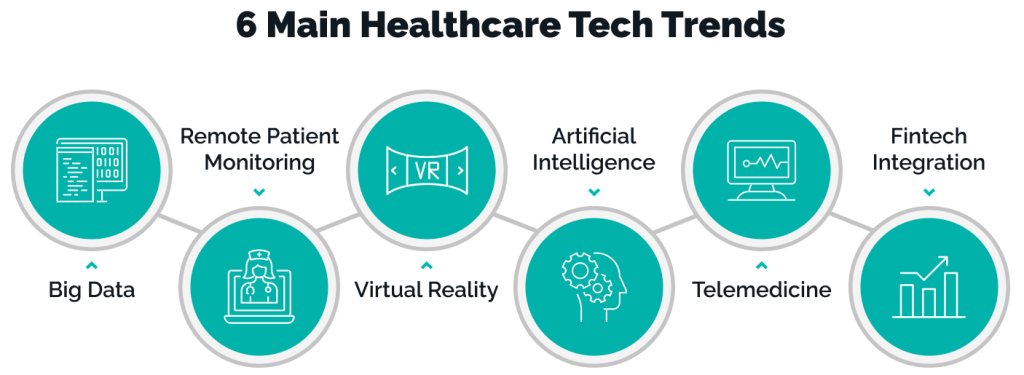
Pillar 5: Leveraging Technology and Data Analytics
Technology is not a panacea, but it is a powerful enabler for optimizing healthcare across multiple domains. From digital records to advanced analytics, technology can enhance efficiency, quality, and patient engagement.
Key Strategies:
- Electronic Health Records (EHR) Optimization:
- Improving usability and reducing clinician documentation burden.
- Ensuring interoperability between different EHR systems and healthcare entities.
- Leveraging EHR data for quality reporting, research, and population health management.
- Integrating clinical decision support tools effectively.
- Telehealth Expansion:
- Utilizing video consultations, remote patient monitoring, and mobile health apps to extend care reach and convenience.
- Integrating telehealth seamlessly into existing care workflows.
- Ensuring equitable access to telehealth services.
- Data Analytics and Artificial Intelligence (AI):
- Using predictive analytics to identify high-risk patients, forecast demand, and optimize resource allocation.
- Applying AI and machine learning to diagnostic imaging, drug discovery, and personalized treatment recommendations.
- Utilizing real-time data dashboards to monitor performance and guide operational decisions.
- Ensuring robust data governance, privacy, and security measures.
- Patient-Facing Technologies:
- Developing user-friendly patient portals and mobile apps.
- Utilizing wearable devices for health tracking and remote monitoring.
- Providing digital tools for health education and self-management.
Strategic implementation and integration of technology are crucial components of modern efforts aimed at optimizing healthcare. Harnessing the power of data is key to understanding performance and driving targeted improvements. The potential for optimizing healthcare through technological innovation is immense.
Pillar 6: Navigating Policy and Systemic Change
While individual organizations can make significant strides, system-wide optimizing healthcare often requires supportive policies and regulatory frameworks. Collaboration between healthcare providers, payers, and government agencies is vital.
Key Strategies:
- Advocating for Value-Based Care Models: Encouraging policies that shift reimbursement away from volume and towards quality, outcomes, and patient experience.
- Promoting Interoperability Standards: Supporting regulations and incentives that mandate or encourage seamless data sharing between different healthcare systems and technologies.
- Integrating Public Health and Healthcare Delivery: Fostering collaboration to address population health needs, social determinants of health, and health equity.
- Streamlining Regulations: Identifying and reducing regulatory burdens that do not add significant value to patient safety or care quality.
- Investing in Health Information Infrastructure: Supporting the development of secure and robust data infrastructure to enable better analytics and information exchange.
Policy provides the scaffolding upon which many efforts for optimizing healthcare are built. Aligning incentives and removing systemic barriers are essential for widespread and sustainable improvement. This systemic approach is vital for truly optimizing healthcare on a larger scale.
Methodologies and Tools for Optimizing Healthcare
Several established methodologies provide frameworks and tools to guide the process of optimizing healthcare:
- Lean Healthcare: Focuses on eliminating waste (muda), improving flow, and maximizing value from the patient’s perspective. Tools include value stream mapping, 5S workplace organization, Kanban systems, and A3 problem-solving.
- Six Sigma: A data-driven methodology aimed at reducing defects and variation in processes. Uses the DMAIC (Define, Measure, Analyze, Improve, Control) cycle and statistical tools.
- Continuous Quality Improvement (CQI): An ongoing cycle of planning, implementing, studying, and acting (PDSA cycles) to make incremental improvements in processes and outcomes.
- Human-Centered Design: Emphasizes understanding the needs and experiences of end-users (patients, clinicians) to design solutions that are effective, usable, and desirable.
- Baldrige Performance Excellence Framework: A comprehensive framework for organizational assessment and improvement across leadership, strategy, customers, measurement, workforce, and operations.
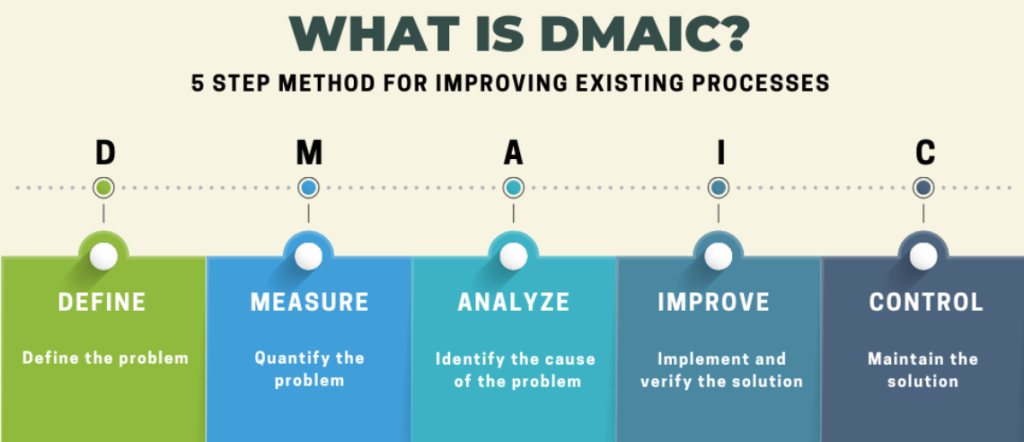
Choosing and applying the right methodologies depends on the specific problem and organizational context, but all aim to provide structured approaches to the complex task of optimizing healthcare.
Challenges and Barriers to Optimizing Healthcare
Despite the clear need and available strategies, optimizing healthcare faces significant hurdles:
- System Complexity: Healthcare systems are intricate networks of providers, payers, regulators, and technologies, making change difficult to implement and coordinate.
- Resistance to Change: Established workflows, cultural norms, and individual habits can create inertia and resistance to new processes or technologies.
- Financial Constraints: Implementing new technologies, training staff, and redesigning processes requires upfront investment, which can be challenging for resource-strapped organizations.
- Data Challenges: Issues with data quality, interoperability, privacy concerns, and the analytical skills needed to interpret data can hinder progress.
- Regulatory Hurdles: Complex and sometimes conflicting regulations can slow down innovation and process improvement.
- Workforce Shortages and Burnout: Lack of sufficient staff and high levels of burnout limit the capacity for change initiatives.
- Health Inequities: Addressing the deep-rooted social and economic factors that drive health disparities requires efforts that extend beyond the traditional healthcare system.
Overcoming these challenges requires persistent leadership, clear communication, stakeholder engagement, and a long-term commitment to the goals of optimizing healthcare.
The Crucial Role of Research and Education in Optimizing Healthcare
Continuous learning and knowledge generation are fundamental to sustained progress. Research informs best practices, identifies emerging challenges, and evaluates the effectiveness of interventions aimed at optimizing healthcare.
- Identifying Best Practices: Research helps determine which clinical treatments, operational processes, and technological applications yield the best results in terms of quality, safety, efficiency, and patient experience.
- Evaluating Interventions: Rigorous evaluation is needed to understand the impact and cost-effectiveness of various initiatives designed for optimizing healthcare.
- Understanding System Dynamics: Research can illuminate the complex interactions within healthcare systems and identify leverage points for improvement.
- Developing New Solutions: Innovation in diagnostics, therapeutics, digital health tools, and care models often stems from dedicated research efforts.
Academia plays a vital role. Students and researchers often need help with a research paper about optimizing healthcare, tackling specific questions about efficiency, quality, or access. Undertaking a dissertation about healthcare delivery allows for in-depth exploration of complex systemic issues, contributing valuable knowledge to the field. PhD Nurse Writer is the go-to dissertation expert. We help students with writing authentic and impactful dissertations about all nursing topics and study areas. Our service covers topic suggestion, dissertation writing, proofreading, editing, formatting and plagiarism removal. Besides, our writing services also cover essays, term papers, TEAS exams, assignments, research papers, case studies and thesis.
The process of writing a paper about optimizing healthcare not only disseminates findings but also helps synthesize complex information and propose actionable solutions. Educational programs can equip future healthcare leaders and professionals with the skills needed for optimizing healthcare, including quality improvement methodologies, data analysis, change management, and systems thinking. This continuous cycle of research, education, and practice is essential for the ongoing journey of optimizing healthcare.
Future Trends in Optimizing Healthcare
The landscape of healthcare is constantly evolving. Several key trends will shape the future of optimizing healthcare:
- Hyper-Personalization: Leveraging genomics, lifestyle data, and AI to tailor prevention strategies and treatments to the individual.
- Predictive and Proactive Care: Using AI and big data to anticipate health issues before they become critical, shifting focus from reactive treatment to proactive wellness.
- Ambient Intelligence: Integrating sensors and AI into the environment (hospitals, homes) to unobtrusively monitor health and assist with care.
- Increased Consumerism: Patients taking a more active role in managing their health and choosing providers, demanding greater transparency and convenience.
- Hospital-at-Home Models: Expanding capabilities to provide acute-level care in the patient’s home, enabled by technology and specialized care teams.
- Focus on Social Determinants: Greater integration of efforts to address social factors like housing, nutrition, and education that significantly impact health outcomes.
- Global Collaboration: Increased sharing of data, best practices, and research findings across borders to tackle global health challenges and accelerate the pace of optimizing healthcare worldwide.
These trends offer exciting possibilities but also present new challenges related to ethics, equity, data privacy, and workforce adaptation. Navigating them successfully will be key to future success in optimizing healthcare.
Conclusion: The Continuous Journey of Optimizing Healthcare
Optimizing healthcare is not a destination but an ongoing, dynamic process. It requires a fundamental shift in mindset – from accepting the status quo to relentlessly pursuing improvement across all dimensions of care. It demands strong leadership, a culture of continuous learning, effective use of data and technology, and genuine collaboration among all stakeholders, especially patients.
The path involves embracing patient-centeredness, rigorously ensuring quality and safety, driving operational efficiency, supporting the vital healthcare workforce, strategically leveraging technology, and advocating for supportive policies. While challenges exist, the methodologies and tools are available, and the potential benefits – improved health outcomes, enhanced patient and provider experiences, greater equity, and sustainable systems – are immense.
From the student seeking help with a research paper about optimizing healthcare to the seasoned executive leading system-wide transformation, everyone has a role to play. The collective commitment to optimizing healthcare is a commitment to a healthier future for individuals and communities everywhere. It is perhaps the most critical undertaking for ensuring the well-being of generations to come, making the continuous effort of optimizing healthcare an essential mission for our time. The future of health depends on our collective will and ability for optimizing healthcare effectively and equitably.





