
Table of Contents
Adult nursing stands as a cornerstone of healthcare systems worldwide, providing essential care to individuals navigating a vast spectrum of health challenges, life stages, and personal circumstances. In an increasingly interconnected and diverse world, the effectiveness of this care hinges significantly on the ability of nurses to understand and respond appropriately to the cultural backgrounds of their patients. This ability is encapsulated in the concept of cultural competence in adult nursing, a dynamic and multifaceted process that goes beyond mere awareness or sensitivity.
It represents a fundamental commitment to providing equitable, respectful, and effective care to all patients, acknowledging that culture profoundly influences health beliefs, practices, communication styles, and responses to illness and treatment. Achieving meaningful cultural competence in adult nursing is not merely an aspirational goal; it is an ethical imperative and a practical necessity for improving patient outcomes and reducing health disparities. Developing and sustaining cultural competence in adult nursing is critical for ensuring that care is patient-centered, holistic, and truly therapeutic.
This article will cover the definition, significance, components, challenges, and strategies associated with fostering cultural competence in adult nursing, highlighting its pivotal role in contemporary healthcare delivery.
What is Cultural Competence in Adult Nursing?
Cultural competence is often described as a set of congruent behaviors, attitudes, and policies that come together in a system, agency, or among professionals, enabling them to work effectively in cross-cultural situations. It involves understanding the impact of cultural differences on patient health values, beliefs, and behaviors. However, cultural competence in adult nursing is more than just possessing knowledge about different cultures; it is an active, ongoing process of self-reflection, learning, and skill development.
Key aspects of this definition include:
- Integration: It’s not a separate skill set but should be integrated into every aspect of nursing care, from assessment to intervention and evaluation.
- Developmental Process: Nurses are not simply ‘competent’ or ‘incompetent’; they exist on a continuum and must continuously strive to improve their cultural competence in adult nursing.
- Patient-Centered: The focus is always on understanding the individual patient within their cultural context, avoiding generalizations or stereotypes.
- Beyond Ethnicity: Culture encompasses more than just race or ethnicity; it includes factors like socioeconomic status, religion, sexual orientation, gender identity, age, disability, and geographic origin. True cultural competence in adult nursing acknowledges this intersectionality.
It is crucial to differentiate cultural competence from related concepts:
- Cultural Awareness: Recognizing that cultural differences exist.
- Cultural Sensitivity: Acknowledging and respecting these differences without assigning judgment (better/worse, right/wrong).
- Cultural Humility: A lifelong commitment to self-evaluation and self-critique, redressing power imbalances, and developing mutually beneficial partnerships with communities on behalf of individuals and defined populations.
While awareness and sensitivity are necessary starting points, cultural competence in nursing demands a deeper level of engagement, requiring nurses to actively use their understanding to adapt their practice and provide tailored, effective care. It necessitates moving beyond tolerance towards active affirmation and skilled adaptation.

Why Cultural Competence in Adult Nursing Matters Profoundly
The rationale for prioritizing cultural competence in adult nursing is multifaceted, touching upon ethical obligations, professional standards, patient safety, and health equity.
- Addressing Health Disparities: Significant disparities in health outcomes persist across different cultural, ethnic, and socioeconomic groups. These disparities are often linked to barriers in accessing care, communication breakdowns, implicit bias among providers, and care plans that do not align with patients’ cultural beliefs or realities. Enhancing cultural competence in adult nursing is a key strategy for mitigating these factors and promoting health equity. Nurses who are culturally competent are better equipped to identify and address the specific needs and barriers faced by diverse patient populations.
- Building Trust and Therapeutic Relationships: Trust is the bedrock of the nurse-patient relationship. Patients are more likely to trust and communicate openly with nurses who demonstrate respect for their cultural background, attempt to understand their perspective, and involve them as active partners in their care. This trust is essential for accurate assessment, effective communication, and patient adherence to treatment. Strong cultural competence in adult nursing directly fosters this trust.
- Improving Patient Safety and Outcomes: Misunderstandings arising from cultural differences can lead to serious patient safety issues. Examples include misinterpreting symptoms described in culturally specific ways, overlooking non-verbal cues, medication errors due to language barriers or misunderstandings about instructions, and adverse reactions to treatments that conflict with traditional remedies or dietary practices. Effective cultural competence in adult nursing helps prevent these errors by promoting clear communication and culturally informed assessments and interventions.
- Enhancing Patient Satisfaction and Adherence: When patients feel understood, respected, and involved in their care, their satisfaction levels increase significantly. They are also more likely to adhere to treatment plans and follow preventative health advice if it aligns with their cultural values and lifestyle. Nurses practicing robust cultural competence in adult nursing contribute directly to a more positive patient experience and better self-management of health conditions.
- Meeting Ethical and Professional Standards: Nursing codes of ethics (e.g., from the American Nurses Association or the International Council of Nurses) emphasize the principles of social justice, respect for autonomy, dignity, and providing care without prejudice. Professional standards and regulatory bodies increasingly mandate culturally competent care. Therefore, developing cultural competence in adult nursing is not just good practice; it is a professional and ethical obligation.
- Navigating Complex Adult Health Needs: Adult patients often present with chronic conditions, complex medical histories, and established beliefs about health and illness shaped by years of cultural experience. They may also be navigating significant life decisions regarding treatment options, palliative care, or end-of-life planning, all heavily influenced by cultural norms. Effective cultural competence in adult nursing is essential for navigating these sensitive and complex situations respectfully and effectively.
Key Components and Models of Cultural Competence in Nursing
Several models have been developed to guide the development and application of cultural competence in healthcare. While models vary, they generally emphasize similar core components crucial for achieving cultural competence in adult nursing. One widely recognized framework is Dr. Josepha Campinha-Bacote’s model, “The Process of Cultural Competence in the Delivery of Healthcare Services,” which outlines five interrelated constructs:
- Cultural Awareness: This involves the process of self-examination and in-depth exploration of one’s own cultural and professional background. It requires nurses to recognize their biases, prejudices, and assumptions about individuals who are different. This introspection is the foundation upon which effective cultural competence in adult nursing is built.
- Self-Reflection: Regularly questioning one’s own values, beliefs, and assumptions.
- Bias Recognition: Identifying personal and systemic biases that could affect patient care.
- Cultural Knowledge: This is the process of seeking and obtaining a sound educational foundation about diverse cultural and ethnic groups. This involves understanding their worldviews, health-related beliefs and practices, disease incidence and prevalence, and treatment efficacy. However, it’s vital to avoid stereotyping; knowledge should serve as a guide, not a rigid template. Acquiring relevant cultural knowledge is central to enhancing cultural competence in adult nursing.
- Specific Beliefs: Learning about common health beliefs, traditional remedies, and views on illness causation.
- Social Determinants: Understanding how factors like poverty, education, and environment intersect with culture to impact health.
- Cultural Skill: This refers to the ability to conduct a culturally sensitive assessment and collect relevant cultural data regarding the patient’s presenting problem, as well as accurately performing a culturally specific physical assessment. This involves adapting communication styles and assessment techniques. Developing these practical abilities demonstrates tangible cultural competence in adult nursing.
- Communication: Using appropriate language, employing interpreters effectively, understanding non-verbal cues.
- Assessment: Incorporating questions about cultural practices, beliefs, preferences, and social support into the standard nursing assessment.
- Cultural Encounters: This encourages healthcare professionals to directly engage in face-to-face interactions with patients from culturally diverse backgrounds. These encounters allow nurses to refine or challenge their existing beliefs and prevent potential stereotyping. Meaningful interactions are vital for the practical application and growth of cultural competence in adult nursing.
- Direct Interaction: Seeking opportunities to care for diverse patients.
- Learning from Experience: Viewing each encounter as a learning opportunity, asking questions respectfully.
- Cultural Desire: This is the motivation of the healthcare professional to want to engage in the process of becoming culturally aware, knowledgeable, skillful, and seeking cultural encounters; it’s distinct from having to. It involves a genuine aspiration to provide culturally responsive care, rooted in compassion and empathy. Cultural desire is the pivotal ‘wanting to’ that drives the journey towards authentic cultural competence in adult nursing.
- Motivation: Possessing a genuine interest in understanding and working with diverse populations.
- Humility: Approaching interactions with humility, acknowledging one doesn’t know everything.
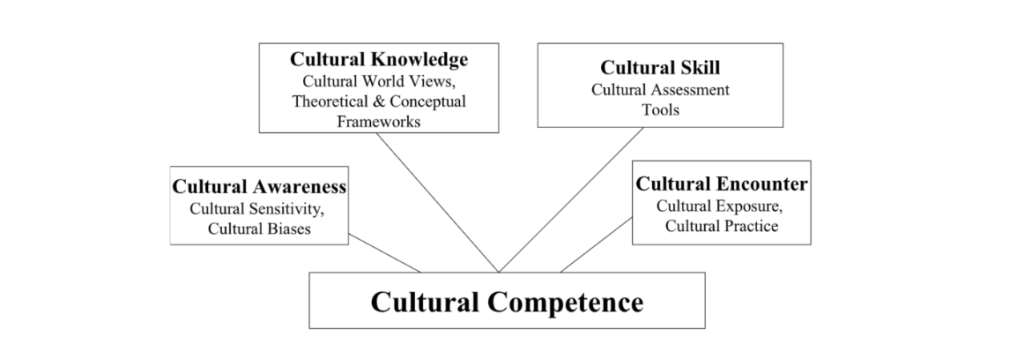
Mastering these components requires ongoing effort and commitment, making cultural competence in adult nursing a continuous journey rather than a destination.
Barriers to Achieving Cultural Competence in Adult Nursing
Despite its recognized importance, achieving widespread cultural competence in adult nursing faces numerous obstacles at individual, institutional, and systemic levels.
- Individual Barriers:
- Stereotyping: Applying preconceived notions or generalizations about a cultural group to an individual patient, ignoring intra-group diversity.
- Prejudice and Discrimination: Holding negative attitudes or beliefs (prejudice) that lead to unfair treatment (discrimination).
- Ethnocentrism: Believing one’s own cultural ways are superior, normal, or right, and judging others accordingly.
- Lack of Awareness: Nurses may be unaware of their own biases or the impact of culture on health.
- Fear and Mistrust: Hesitancy to ask culturally relevant questions for fear of offending the patient.
- Systemic and Institutional Barriers:
- Inadequate Education and Training: Nursing curricula may not sufficiently integrate cultural competence in adult nursing, or continuing education opportunities may be limited.
- Language Barriers: Lack of access to qualified medical interpreters or reliance on family members (which can compromise confidentiality and accuracy).
- Time Constraints: Heavy workloads and staffing shortages can limit the time available for thorough, culturally sensitive assessments and communication.
- Lack of Diversity in Workforce: A homogenous nursing workforce may struggle to understand and meet the needs of a diverse patient population.
- Organizational Culture: Healthcare systems may lack policies, resources, or leadership commitment to support cultural competence in adult nursing.
- Focus on Biomedical Model: Over-reliance on a purely biomedical approach can overshadow the psychosocial and cultural dimensions of health and illness.
- Patient-Related Factors:
- Mistrust of Healthcare System: Past experiences of discrimination or culturally insensitive care can make patients hesitant to engage openly.
- Communication Challenges: Patients may feel uncomfortable expressing cultural needs or questioning providers.
Overcoming these barriers requires a multi-pronged approach involving individual commitment, educational reform, and organizational change to truly embed cultural competence in adult nursing into the fabric of healthcare.
How to Enhance Cultural Competence in Adult Nursing
Fostering cultural competence in adult nursing is an active process requiring deliberate strategies and ongoing commitment from individual nurses, educators, and healthcare organizations.
- Education and Training:
- Curriculum Integration: Nursing schools must embed cultural competence principles throughout the curriculum, not just in isolated modules.
- Continuing Education: Hospitals and healthcare systems should offer regular workshops, seminars, and online courses focused on cultural competence in adult nursing, addressing specific local populations and emerging needs.
- Simulation: Using simulated patient encounters with diverse cultural scenarios can provide safe practice opportunities.
- Self-Reflection and Bias Awareness:
- Journalling: Regularly reflecting on clinical encounters, identifying personal reactions and potential biases.
- Implicit Bias Testing: Utilizing tools like the Implicit Association Test (IAT) to uncover unconscious biases.
- Seeking Feedback: Asking trusted colleagues or mentors for feedback on cross-cultural interactions. This continuous self-assessment is vital for cultural competence in adult nursing.
- Exposure and Diverse Experiences:
- Seeking Diverse Assignments: Voluntarily working in settings with diverse patient populations.
- Community Engagement: Participating in community health fairs or events in diverse neighborhoods.
- Learning from Patients: Viewing patients as experts on their own culture and experiences; asking open-ended questions respectfully.
- Developing Cross-Cultural Communication Skills:
- Active Listening: Paying close attention to verbal and non-verbal cues, seeking clarification.
- Using Plain Language: Avoiding medical jargon and ensuring understanding.
- Working with Interpreters: Learning best practices for using professional medical interpreters effectively. Mastering communication is key to practical cultural competence in adult nursing.
- Utilizing Resources:
- Cultural Brokers: Engaging individuals who can mediate between the healthcare system and the patient’s culture.
- Culturally Specific Materials: Using patient education materials available in multiple languages and formats that are culturally appropriate.
- Organizational Resources: Leveraging resources provided by the healthcare institution, such as diversity departments or cultural liaisons.
- Adopting Cultural Humility:
- Lifelong Learning: Recognizing that cultural competence is an ongoing journey, not a final achievement.
- Acknowledging Limitations: Being open about what one does not know and being willing to learn.
- Respecting Patient Expertise: Understanding that the patient is the expert on their own life, beliefs, and values. This humility underpins genuine cultural competence in adult nursing.
- Organizational Support:
- Policies and Procedures: Implementing policies that mandate and support culturally competent care (e.g., access to interpreters).
- Diverse Workforce: Actively recruiting and retaining a nursing workforce that reflects the diversity of the patient population.
- Leadership Commitment: Ensuring that hospital leadership champions and invests in cultural competence in adult nursing initiatives.
These strategies, when implemented consistently, can significantly enhance the capacity of nurses and healthcare systems to provide truly patient-centered, culturally responsive care. Improving cultural competence in adult nursing requires this multifaceted approach.
Research and Education in Cultural Competence in Adult Nursing
Continuous improvement in cultural competence in adult nursing relies heavily on ongoing research and robust educational initiatives. Research is needed to better understand the specific cultural needs of diverse populations, evaluate the effectiveness of cultural competence interventions, and identify best practices. Scholars undertaking a dissertation about cultural competence in adult nursing, for example, contribute valuable knowledge by exploring nuances in specific cultural groups, evaluating training programs, or developing new assessment tools. Such academic work helps refine theoretical models and provides evidence-based strategies for practice and education.
Furthermore, integrating comprehensive training on cultural competence in adult nursing into undergraduate and graduate nursing programs is essential. This education should go beyond superficial overviews of different cultures and focus on developing skills in self-reflection, communication, assessment, and cultural humility. It should also address systemic issues like bias and health disparities.
Many students and researchers find the topic complex and often seek help with research about cultural competence in adult nursing to navigate the extensive literature and methodologies effectively. At PhD Nurse Writer, we can help you with professional dissertation research, writing, proofreading, editing, formatting and plagiarism removal. We have highly experienced researchers and skilled writers to deliver an impactful essay, research paper, case study, thesis or dissertation about cultural competence in adult nursing.
Conclusion: Embracing Cultural Competence as Foundational Nursing Practice
In conclusion, cultural competence in adult nursing is far more than a buzzword or an optional add-on; it is an essential component of safe, ethical, and effective nursing care in the 21st century. As patient populations become increasingly diverse, the ability of nurses to understand, respect, and respond effectively to cultural differences is paramount. It directly impacts patient safety, trust, adherence, satisfaction, and ultimately, health outcomes. Achieving health equity requires a concerted effort to address the barriers that prevent culturally competent care, many of which are deeply embedded within healthcare systems.
The journey towards enhanced cultural competence in adult nursing involves a commitment to lifelong learning, starting with cultural awareness and humility, building cultural knowledge and skill through education and experience, and actively seeking meaningful cultural encounters. It requires nurses to critically examine their own biases and assumptions and to approach each patient as an individual within their unique cultural context. While individual nurses bear responsibility, healthcare organizations and educational institutions play a critical role in fostering an environment that supports and demands cultural competence in adult nursing through training, policies, resources, and leadership.
The development of strong cultural competence in adult nursing benefits not only diverse patient populations but also enriches the nursing profession itself, fostering greater empathy, understanding, and professional satisfaction. It transforms nursing practice from a standardized application of procedures to a truly holistic and patient-centered art and science. Ultimately, embracing and prioritizing cultural competence in adult nursing is fundamental to fulfilling the core mission of nursing: to provide compassionate, high-quality care to all individuals, regardless of their background, ensuring dignity and respect in every interaction.
The future of excellent adult nursing care is inextricably linked to the consistent practice of cultural competence in adult nursing. Therefore, the pursuit of cultural competence in adult nursing must remain a central focus for every nurse, educator, researcher, and healthcare leader. It is the indispensable heart of modern, equitable healthcare.





