
Table of Contents
The healthcare landscape of 2025 continues to grapple with a persistent and pervasive crisis: nurse burnout and mental health deterioration among its most vital workforce. Nurses, the backbone of patient care, are facing unprecedented pressures that significantly impact their well-being, the quality of care they provide, and the stability of healthcare systems globally.
This comprehensive guide dissects the multifaceted issue of nurse burnout and mental health, offering insights into its causes, symptoms, consequences, and crucially, forward-looking strategies for prevention, intervention, and support. Addressing nurse burnout and mental health is no longer optional; it’s an imperative for a sustainable and compassionate healthcare future.
Understanding the Dual Crisis: Nurse Burnout and Mental Health
It’s essential to distinguish between and understand the interplay of burnout and broader mental health conditions, though they often overlap and exacerbate each other. The crisis of nurse burnout and mental health demands a nuanced understanding.
What is Nurse Burnout?
Burnout, as defined by the World Health Organization, is an occupational phenomenon resulting from chronic workplace stress that has not been successfully managed. It is characterized by three primary dimensions:
- Emotional Exhaustion: Feeling emotionally drained, depleted, and unable to give more of oneself at a psychological level. This is a core component when discussing nurse burnout and mental health.
- Depersonalization or Cynicism: Developing a detached, indifferent, or cynical attitude towards one’s work, colleagues, and patients. This detachment is a significant warning sign related to nurse burnout and mental health.
- Reduced Personal Accomplishment: Experiencing a sense of inefficacy, a lack of achievement, and declining productivity or competence in one’s work.
Mental Health in Nursing:
Beyond burnout, nurses are at a heightened risk for various mental health conditions, including:
- Anxiety Disorders: Persistent worry, fear, and unease related to work pressures, patient outcomes, or personal safety.
- Depression: Characterized by persistent sadness, loss of interest, fatigue, and changes in sleep or appetite. The link between chronic stress and depression makes understanding nurse burnout and mental health even more critical.
- Post-Traumatic Stress Disorder (PTSD): Arising from exposure to traumatic events, such as patient deaths, medical emergencies, or workplace violence, which are unfortunately common in nursing.
- Compassion Fatigue: A state of emotional and physical exhaustion leading to a diminished ability to empathize or feel compassion for others, often described as the “cost of caring.” This is intrinsically linked to the challenges of nurse burnout and mental health.
The interconnectedness of nurse burnout and mental health means that one can often trigger or worsen the other, creating a vicious cycle that is difficult to break without targeted interventions.
The Scope of the Problem in 2025: Alarming Statistics and Trends
By 2025, the data paints a stark picture of the ongoing struggle with nurse burnout and mental health. Several factors have contributed to the current state:
- Lingering Effects of the Pandemic: The COVID-19 pandemic placed an unprecedented and prolonged strain on healthcare systems and nurses, the repercussions of which are still deeply felt. This has undeniably worsened the state of nurse burnout and mental health.
- Chronic Staffing Shortages: An aging nursing workforce, insufficient new graduates entering high-stress specialties, and high turnover rates (often due to burnout itself) have led to persistent understaffing.
- Increased Patient Acuity and Complexity: Patients in hospital settings are often sicker and require more intensive care, increasing the cognitive and emotional load on nurses.
- Administrative Burdens: Excessive documentation, electronic health record (EHR) complexities, and non-clinical tasks detract from direct patient care and add to frustration, contributing significantly to issues of nurse burnout and mental health.
Key Statistics (Projected/Observed by 2025):
- Surveys consistently indicate that over 60-70% of nurses report symptoms of burnout.
- A significant percentage (around 30-40%) of nurses report symptoms of anxiety or depression.
- Suicidal ideation among nurses remains alarmingly higher than in the general population, highlighting the severe end of the nurse burnout and mental health spectrum.
- Nurse turnover rates, driven by these issues, are projected to cost healthcare systems billions annually.
The pervasive nature of nurse burnout and mental health issues necessitates a systemic response.
Unpacking the Root Causes of Nurse Burnout and Mental Health Challenges
Addressing nurse burnout and mental health effectively requires a deep dive into its myriad causes, which can be broadly categorized into systemic/organizational factors and individual factors.
Systemic and Organizational Factors:
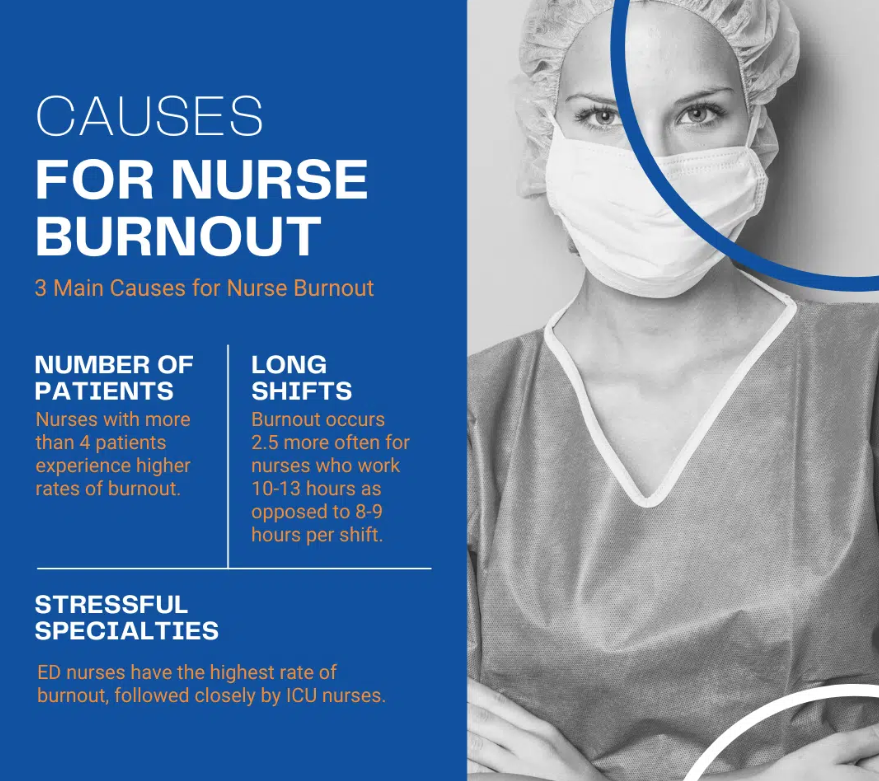
- Excessive Workload and Unsafe Staffing Ratios:
- High patient-to-nurse ratios.
- Frequent overtime (mandatory or coerced).
- Insufficient breaks and rest periods.
- Lack of Control and Autonomy:
- Limited input into decision-making processes.
- Rigid protocols that don’t allow for professional judgment.
- Inadequate influence over scheduling.
- Insufficient Support and Resources:
- Lack of managerial support and recognition.
- Poor teamwork or interprofessional conflict.
- Inadequate supplies, equipment, or ancillary staff.
- Limited access to mental health support services specifically tailored for healthcare professionals.
- Workplace Environment:
- Exposure to trauma, death, and ethical dilemmas.
- Workplace violence and aggression (from patients or families).
- A culture that stigmatizes seeking help for nurse burnout and mental health issues.
- Poor communication and lack of transparency from leadership.
- Administrative Burdens:
- Time-consuming EHR documentation.
- Non-nursing tasks diverting time from patient care.
- Inadequate Compensation and Benefits:
- Pay not commensurate with workload, stress, and responsibility.
- Limited access to comprehensive mental health coverage.
Individual and Professional Factors:
- High Levels of Empathy and Compassion: While virtues, these can lead to compassion fatigue if not managed.
- Perfectionism and High Self-Expectation: Nurses often hold themselves to exceptionally high standards.
- Difficulty Setting Boundaries: Challenges in saying “no” to extra shifts or responsibilities.
- Coping Mechanisms: Resorting to unhealthy coping strategies (e.g., substance use) rather than seeking support for nurse burnout and mental health.
- Lack of Work-Life Balance: Difficulty disconnecting from work and prioritizing personal well-being.
- Moral Distress: Arising when nurses know the ethically correct action to take but are constrained from taking it.
Understanding these multifaceted causes is the first step in developing targeted solutions for nurse burnout and mental health.
The Consequences of Unaddressed Nurse Burnout and Mental Health
The failure to adequately address nurse burnout and mental health has profound negative consequences across multiple levels:
For Nurses:
- Deterioration in Physical Health: Increased risk of cardiovascular disease, weakened immune system, sleep disorders, headaches, and gastrointestinal problems.
- Worsening Mental Health: Progression to clinical depression, anxiety disorders, PTSD, increased risk of substance abuse, and suicidal ideation. The trajectory of nurse burnout and mental health can be devastating.
- Decreased Job Satisfaction: Leading to disillusionment with the nursing profession.
- Increased Absenteeism and Presenteeism: Being physically present but mentally disengaged.
- Career Abandonment: Nurses leaving the profession altogether, exacerbating staffing shortages.
For Patients:
- Compromised Patient Safety: Increased risk of medical errors, medication mistakes, and hospital-acquired infections.
- Reduced Quality of Care: Less attentive care, decreased patient satisfaction, and poorer communication.
- Negative Patient Experiences: Patients may perceive nurses as uncaring or detached.
For Healthcare Organizations:
- Increased Staff Turnover: High costs associated with recruitment, hiring, and training new nurses.
- Decreased Productivity: Burned-out staff are less efficient and effective.
- Financial Strain: Costs related to errors, litigation, and reputational damage.
- Lower HCAHPS Scores (Hospital Consumer Assessment of Healthcare Providers and Systems): Impacting reimbursement and public perception.
The ripple effects underscore why tackling nurse burnout and mental health is a societal imperative.
Recognizing the Warning Signs: Early Detection of Nurse Burnout and Mental Health Issues
Early recognition is crucial for timely intervention. Both individuals and organizations should be vigilant for signs of nurse burnout and mental health challenges.
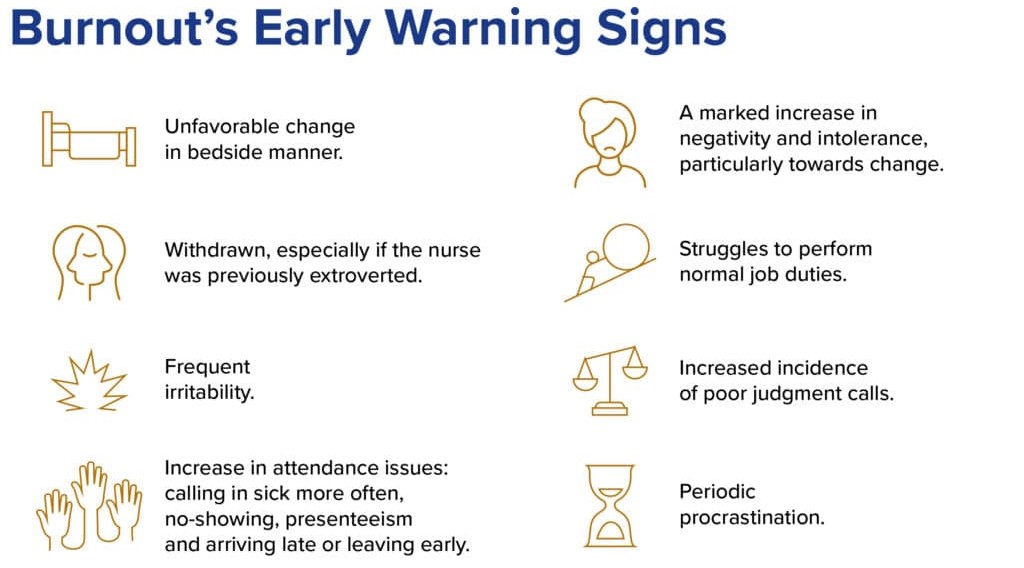
Individual Warning Signs:
- Emotional:
- Feeling overwhelmed, irritable, or anxious most of a shift.
- Loss of enjoyment in work or previously enjoyed activities.
- Increased cynicism or negativity.
- Feeling emotionally numb or detached from patients.
- A sense of dread before going to work.
- Physical:
- Chronic fatigue, even after rest.
- Frequent headaches or muscle pain.
- Changes in appetite or sleep patterns.
- Lowered immunity, frequent illnesses.
- Behavioral:
- Increased absenteeism or tardiness.
- Procrastination and difficulty concentrating.
- Social withdrawal from colleagues or loved ones.
- Increased use of alcohol, drugs, or caffeine.
- Making more errors or near misses.
Organizational Red Flags:
- High staff turnover rates.
- Increased sick leave usage.
- Elevated rates of patient complaints or safety incidents.
- Low morale and frequent staff conflicts.
- Difficulty recruiting and retaining nurses.
- A palpable atmosphere of stress and negativity.
Addressing these signs promptly can mitigate the progression of serious nurse burnout and mental health problems.
Strategies for Preventing and Mitigating Nurse Burnout and Mental Health
Combating the crisis of nurse burnout and mental health requires a comprehensive strategy involving individual nurses, healthcare organizations, and policymakers.
Individual-Level Strategies:
- Prioritize Self-Care (Beyond Bubble Baths):
- Adequate Sleep: Aim for 7-9 hours of quality sleep.
- Nutrition: Maintain a balanced diet.
- Regular Exercise: Physical activity is a known stress reliever.
- Mindfulness and Meditation: Practices to reduce stress and improve focus.
- Hobbies and Interests: Engage in activities outside of work that bring joy and relaxation.
- Set Healthy Boundaries:
- Learn to say “no” to extra shifts or responsibilities when feeling overwhelmed.
- Protect personal time and disconnect from work.
- Develop Healthy Coping Mechanisms:
- Journaling, creative expression, spending time in nature.
- Avoid reliance on substances.
- Seek Social Support:
- Connect with supportive colleagues, friends, and family.
- Participate in peer support groups.
- Professional Development and Growth:
- Seek opportunities for continuous learning and skill development.
- Consider mentorship or coaching.
- Access Professional Help:
- Utilize Employee Assistance Programs (EAPs).
- Seek therapy or counseling without shame. Recognizing the need for professional help is key in managing nurse burnout and mental health.
Organizational-Level Strategies (The Foundation for Change):
- Ensure Safe Staffing Levels:
- Implement and enforce evidence-based nurse-to-patient ratios.
- Utilize acuity-based staffing models.
- Invest in float pools and flexible staffing options. This is fundamental to improving nurse burnout and mental health.
- Foster a Supportive Work Environment:
- Visible and Supportive Leadership: Managers who actively listen, advocate for their staff, and promote well-being.
- Promote Teamwork and Collaboration: Create a culture of mutual respect and support.
- Zero Tolerance for Workplace Violence: Implement robust prevention and response strategies.
- Destigmatize Mental Health: Encourage open conversations and make it safe to seek help for nurse burnout and mental health.
- Provide Robust Mental Health Resources:
- Easily accessible and confidential counseling services.
- Peer support programs and wellness champions.
- Resilience training workshops.
- Dedicated quiet rooms or “recharge rooms” for staff.
- Reduce Administrative Burden:
- Streamline documentation processes (EHR optimization).
- Delegate non-nursing tasks to appropriate support staff.
- Invest in technology that genuinely aids, not hinders, workflow.
- Empower Nurses and Promote Autonomy:
- Involve nurses in decision-making (shared governance models).
- Provide opportunities for professional growth and leadership.
- Recognize and reward nurses for their contributions.
- Promote Work-Life Balance:
- Flexible scheduling options.
- Ensure adequate break times and paid time off.
- Discourage a culture of excessive overtime.
- Invest in Ergonomics and Physical Safety:
- Provide proper lifting equipment and safe patient handling policies.
- Ensure a physically comfortable and safe work environment.
Implementing these organizational changes is paramount for a sustainable impact on nurse burnout and mental health.
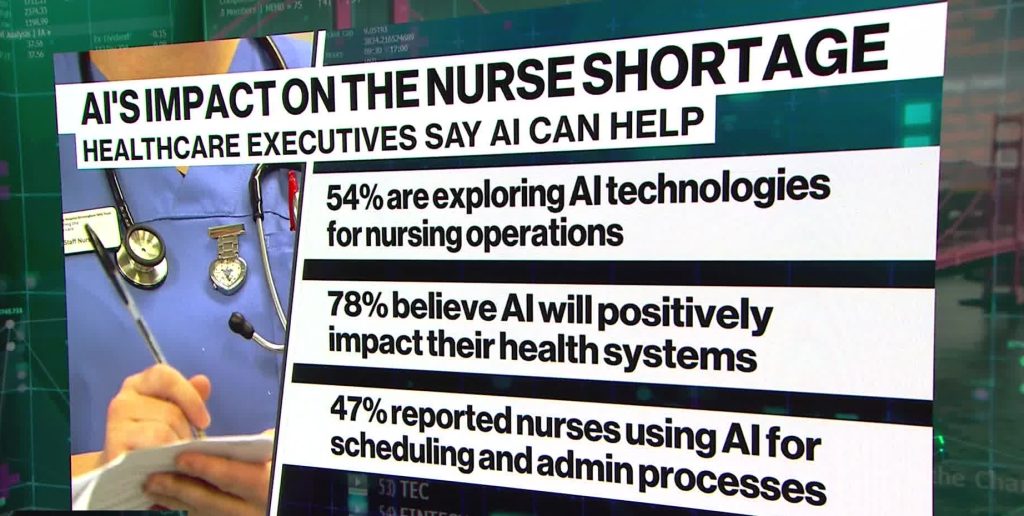
The Role of Technology and Innovation in 2025
By 2025, technology offers both potential solutions and new challenges regarding nurse burnout and mental health.
- Potential Benefits:
- AI and Automation: Can reduce administrative tasks (e.g., AI-powered charting, predictive analytics for staffing).
- Telehealth for Mental Health Support: Increased accessibility to therapists and counselors for nurses.
- Wearable Technology: Monitoring stress levels and promoting well-being interventions.
- Virtual Reality (VR): For stress reduction exercises or empathy training.
- Communication Platforms: Improved team communication and coordination.
- Potential Pitfalls:
- Increased Scrutiny and Surveillance: Technology can sometimes feel intrusive.
- Information Overload: Constant alerts and data can add to cognitive burden.
- Learning Curve and Usability Issues: Poorly designed tech can increase frustration.
The ethical and practical integration of technology must prioritize the well-being of nurses to positively impact nurse burnout and mental health.
Research and Advocacy: Paving the Way Forward
Continuous research is vital to deepen our understanding and refine interventions for nurse burnout and mental health. Many students and academics focus their dissertation about nurse burnout and mental health or research paper about nurse burnout and mental health on these pressing topics, contributing valuable insights.
For those undertaking such demanding academic work, nursing paper writing services from PhD Nurse Writer can offer support in structuring and articulating complex findings, ensuring that valuable research reaches a wider audience and informs practice. We can help you with topic suggestion, paper writing, proofreading, editing, formatting and plagiarism removal. Besides PhD papers, we also assist students with writing essays, research papers, term papers, assignments, case studies and thesis.
Areas for Future Research and Advocacy:
- Long-term impact of interventions on nurse burnout and mental health.
- Effectiveness of specific organizational models in promoting well-being.
- The role of policy and legislation in mandating safe staffing and mental health support.
- Developing culturally sensitive interventions for diverse nursing populations.
- Advocacy for increased funding for nursing education, mental health services, and research into nurse burnout and mental health.
Topic Ideas about Nurse Burnout and Mental Health
The pervasive issue of nurse burnout and mental health continues to challenge healthcare systems globally. To foster meaningful change, deeper exploration into specific facets of this crisis is essential. Here are four vital topic ideas for further investigation and discussion.
Understanding the Core Issues
Delving into the causes and consequences provides a foundational understanding necessary to address nurse burnout and mental health.
- Systemic Factors vs. Individual Burden: Analyze how organizational issues like chronic understaffing, excessive workloads, and inadequate administrative support predominantly drive burnout, rather than individual resilience levels.
- The Impact on Patient Care Quality: Investigate the direct correlation between compromised nurse burnout and mental health and its effects on patient safety, medical errors, and overall healthcare outcomes.
Forging Pathways to Well-being
Identifying and implementing effective solutions is crucial for improving the landscape of nursing.
- Effective Support Systems and Interventions: Explore evidence-based strategies such as accessible mental health services, robust peer support programs, and leadership training focused on creating psychologically safe environments.
- Policy, Advocacy, and Cultural Shifts: Examine the role of policy reform, strong professional advocacy, and organizational culture changes in creating sustainable improvements to tackle widespread nurse burnout and mental health.
Seeking Help: Resources and Support Systems
It is a sign of strength, not weakness, to seek help when struggling with nurse burnout and mental health.
- Employee Assistance Programs (EAPs): Often the first point of contact for confidential support.
- Professional Organizations: Many nursing associations (e.g., ANA, AACN) offer resources and support networks.
- Mental Health Helplines and Crisis Lines: National and local resources for immediate support.
- Therapists and Counselors: Specializing in healthcare professionals or trauma.
- Peer Support Groups: Connecting with others who understand the unique challenges of nursing.
- Online Forums and Communities: Safe spaces for anonymous support and sharing.
No nurse should feel they have to navigate the complexities of nurse burnout and mental health alone.
Conclusion: A Call to Action for 2025 and Beyond
The crisis of nurse burnout and mental health is not an insurmountable challenge, but it demands urgent, sustained, and collective action. By 2025, the narrative must shift from simply acknowledging the problem to actively implementing and embedding solutions at every level. Healthcare organizations must invest in their nursing workforce as their most valuable asset, creating cultures of safety, support, and respect. Individual nurses must be empowered with tools and resources to protect their own well-being. Policymakers must enact legislation that supports safe working conditions.
The future of healthcare hinges on the well-being of its caregivers. Prioritizing nurse burnout and mental health is not just an ethical imperative; it is a strategic necessity for ensuring high-quality patient care, retaining a skilled nursing workforce, and building resilient healthcare systems capable of meeting the challenges of tomorrow. Let 2025 be a turning point where the focus on nurse burnout and mental health translates into tangible, lasting improvements for nurses everywhere. The conversation around nurse burnout and mental health must continue, leading to concrete actions that safeguard these invaluable professionals. Only then can we truly heal the healers and, in turn, heal our healthcare systems. The commitment to addressing nurse burnout and mental health must be unwavering.





