Table of Contents
In the ever-evolving landscape of healthcare, the imperative to deliver the highest quality, safest, and most effective patient care is paramount. Central to achieving this goal is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. This is the essence of evidence-based practice in nursing. For nurses, who are at the forefront of patient care, understanding and implementing evidence-based practice in nursing is not just a professional responsibility but a cornerstone of excellent nursing.
This comprehensive guide aims to demystify evidence-based practice in nursing, explore its components, benefits, challenges, and provide practical steps for its integration into daily nursing routines.
What Exactly is Evidence-Based Practice in Nursing?
Evidence-based practice in nursing (often shortened to EBP nursing or simply EBP) is a problem-solving approach to clinical decision-making that incorporates the best available scientific evidence with the clinician’s expertise and the patient’s unique values and circumstances. It’s a departure from tradition-based or intuition-only practices, advocating for a more systematic and validated approach to care.
The core idea behind evidence-based practice in nursing is to close the gap between what is known (research) and what is done (practice), ensuring that nursing care is based on the most current, valid, and relevant findings. This commitment to evidence-based practice in nursing ultimately elevates the standard of care and patient outcomes.
Key Components of Evidence-Based Practice in Nursing:
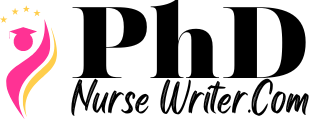
The successful application of evidence-based practice in nursing hinges on the integration of three fundamental components:
- Best Research Evidence: This refers to clinically relevant research, often from medicine and the nursing sciences, that has been conducted using sound methodology. This includes systematic reviews, meta-analyses, randomized controlled trials (RCTs), and other robust study designs. The quality and applicability of this evidence are crucial for effective evidence-based practice in nursing.
- Clinical Expertise: This encompasses the nurse’s cumulated experience, knowledge, and clinical skills. A nurse’s ability to perform a thorough patient assessment, interpret clinical data, and make informed judgments is vital. Clinical expertise allows the nurse to tailor the research evidence to the individual patient within the context of evidence-based practice in nursing.
- Patient Values and Preferences: Each patient is unique, with their own personal, cultural, and religious values, preferences, expectations, and concerns. Evidence-based practice in nursing demands that these individual factors are respected and incorporated into the care plan. Shared decision-making, where the patient is an active participant in their care, is a hallmark of this component.
A fourth component, often implicitly included, is healthcare resources and clinical context. The realities of the healthcare setting, including staffing levels, available equipment, organizational culture, and financial constraints, can influence how evidence-based practice in nursing is implemented.
The Five Steps of Evidence-Based Practice in Nursing (The 5 A’s)
To effectively implement evidence-based practice in nursing, nurses typically follow a systematic process, often summarized as the “5 A’s”:
- Ask: Formulate a clear, answerable clinical question.
- This is the foundational step in evidence-based practice in nursing.
- The PICO(T) format is commonly used:
- Patient/Population/Problem: Who is the patient or group? What is their condition?
- Intervention: What specific intervention, treatment, or diagnostic test is being considered?
- Comparison: What is the main alternative to compare with the intervention (e.g., standard care, another treatment, placebo)?
- Outcome: What is the desired effect or result you hope to achieve or avoid?
- **(T)**ime (optional): What is the timeframe for the intervention or outcome?
- Example: “In adult patients (P) undergoing abdominal surgery (I), does early ambulation (C) compared to bed rest (O) reduce the length of hospital stay (T)?”
- Acquire: Systematically search for the best available evidence.
- This involves identifying relevant research articles from reputable databases and sources.
- Key resources include:
- Cochrane Library (systematic reviews)
- PubMed/MEDLINE
- CINAHL (Cumulative Index to Nursing and Allied Health Literature)
- Joanna Briggs Institute (JBI)
- Professional nursing organization websites
- Developing effective search strategies using keywords and MeSH terms is crucial for efficient acquisition in evidence-based practice in nursing.
- Appraise: Critically evaluate the evidence for its validity, reliability, and applicability.
- Not all research is created equal. Nurses must assess the quality of the studies found.
- Key considerations include:
- Study design (Is it appropriate for the question? RCTs are often considered high-level evidence for intervention questions).
- Sample size and characteristics.
- Control of bias.
- Statistical significance and clinical significance of the results.
- Relevance to your patient population and clinical setting.
- Critical appraisal tools and checklists (e.g., CASP tools) can guide this process, which is integral to evidence-based practice in nursing.
- Apply: Integrate the appraised evidence with clinical expertise and patient preferences to make a clinical decision and implement the change.
- This is where the three core components of evidence-based practice in nursing converge.
- It involves discussing the evidence with the patient, considering their values, and using clinical judgment to determine the best course of action.
- Implementation may involve developing new protocols, educating staff, and securing necessary resources.
- Assess/Audit: Evaluate the outcomes of the practice change.
- After implementing the evidence-based intervention, it’s essential to monitor its impact.
- Did the change lead to the desired outcomes? Were there any unintended consequences?
- This step provides feedback, helps refine the practice, and contributes to the ongoing cycle of evidence-based practice in nursing. Data collection and analysis are key here.
Benefits of Evidence-Based Practice in Nursing
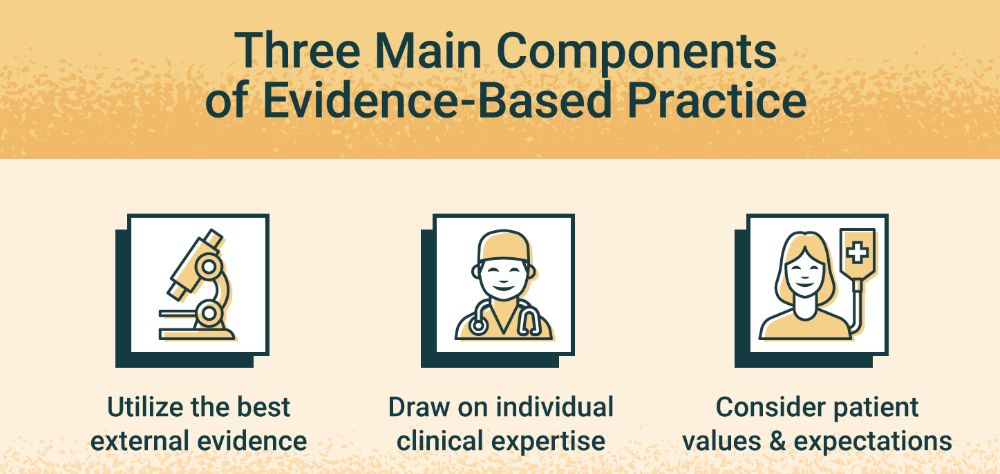
Embracing evidence-based practice in nursing brings a multitude of advantages for patients, nurses, and the healthcare system as a whole:
- Improved Patient Outcomes: This is the primary goal. Care based on rigorous research is more likely to be effective, leading to better health, reduced complications, shorter hospital stays, and improved patient satisfaction.
- Enhanced Quality and Safety of Care: Evidence-based practice in nursing helps standardize care based on proven methods, reducing variability and errors, and promoting patient safety.
- Increased Nurse Satisfaction and Empowerment: When nurses are equipped with the knowledge and skills to engage in evidence-based practice in nursing, they feel more confident, autonomous, and professional. It allows them to advocate effectively for their patients.
- Greater Accountability and Transparency: Decisions are based on evidence rather than solely on tradition or opinion, making the rationale for care more transparent and justifiable.
- Cost-Effectiveness: By implementing interventions that are proven effective, evidence-based practice in nursing can reduce unnecessary treatments, prevent complications, and shorten hospital stays, leading to more efficient use of healthcare resources.
- Professional Development: Engaging in evidence-based practice in nursing promotes critical thinking, lifelong learning, and keeps nurses abreast of the latest advancements in their field.
- Advancement of the Nursing Profession: It solidifies nursing as a science-based profession, contributing to its credibility and influence within the interdisciplinary healthcare team. The rigorous nature of evidence-based practice in nursing strengthens this perception.
Examples of Topics about Evidence-Based Practice in Nursing
Evidence-based practice in nursing (EBP) is no longer a buzzword but a fundamental approach to delivering high-quality, safe, and effective patient care. Exploring compelling aspects of EBP reveals its profound impact on the nursing profession and patient well-being.
1. Enhancing Patient Outcomes and Safety
At its core, EBP aims to improve what matters most: patient health. By moving away from tradition-based care to practices validated by rigorous research, nurses can significantly enhance outcomes.
- Reduced Complications: Implementing evidence-based protocols for infection control (e.g., hand hygiene, catheter care) directly lowers rates of hospital-acquired infections.
- Improved Symptom Management: Research guides best practices for pain assessment and management, leading to better patient comfort and faster recovery.
- Decreased Adverse Events: EBP strategies for fall prevention or medication administration help minimize risks and improve patient safety.
2. Bridging the Research-to-Practice Gap
A significant challenge in healthcare is translating research findings into routine clinical practice. Evidence-based practice in nursing actively seeks to close this gap.
- Systematic Reviews: Nurses learn to access and appraise systematic reviews and meta-analyses, which synthesize multiple studies to provide strong evidence.
- Clinical Guidelines: EBP encourages the development and use of clinical guidelines derived from robust research, offering clear pathways for care.
- Implementation Science: This growing field explores effective strategies to encourage the adoption of evidence-based interventions within complex healthcare settings.
3. Fostering a Culture of Inquiry and Professional Growth
Adopting EBP cultivates an environment where questioning, critical thinking, and continuous learning are valued. This not only benefits patients but also promotes professional development among nurses.
- Lifelong Learning: EBP necessitates that nurses stay updated with current research, fostering a commitment to ongoing education.
- Empowerment: When nurses are equipped to find, appraise, and apply evidence, they feel more confident and empowered in their clinical decision-making.
- Interprofessional Collaboration: EBP often involves collaboration with other healthcare professionals to evaluate and implement best practices, strengthening teamwork. Promoting evidence-based practice in nursing requires strong leadership and organizational support.
4. Addressing Healthcare Costs and Efficiency
While patient care is paramount, the economic realities of healthcare cannot be ignored. EBP can contribute to more efficient and cost-effective care.
- Reducing Unnecessary Interventions: By focusing on practices proven to be effective, EBP can help eliminate outdated or ineffective treatments, saving resources.
- Shortening Hospital Stays: Improved outcomes, such as quicker recovery and fewer complications, can lead to shorter lengths of stay.
- Optimizing Resource Allocation: Evidence can guide decisions on the most effective use of staffing, supplies, and technology.
Ultimately, embracing evidence-based practice in nursing empowers nurses to deliver the highest quality care, grounded in science, leading to better outcomes for patients and a more dynamic, fulfilling profession.
Barriers to Implementing Evidence-Based Practice in Nursing
Despite its clear benefits, the widespread adoption of evidence-based practice in nursing faces several hurdles:
- Lack of Time: Nurses often have demanding workloads, making it difficult to find time to search for, appraise, and implement evidence.
- Limited Access to Resources: Access to research databases, full-text articles, and internet facilities can be restricted in some settings.
- Insufficient Knowledge and Skills: Many nurses may not have received adequate training in EBP processes, including literature searching, critical appraisal, and research interpretation. This is where seeking “help with a paper about evidence-based practice in nursing” or engaging in “nursing research paper writing” courses can be beneficial for students and practicing nurses alike.
- Organizational Culture and Resistance to Change: Traditional practices can be deeply entrenched. A lack of support from management, resistance from colleagues, or a perception that EBP is “too academic” can hinder implementation.
- Overwhelming Amount of Information: The sheer volume of published research can be daunting, making it challenging to identify the most relevant and high-quality evidence.
- Difficulty Understanding Research: Statistical jargon and complex research methodologies can be intimidating for some nurses.
- Lack of Authority to Change Practice: Nurses may feel they lack the autonomy or authority to implement changes, even when supported by evidence.
- Patient Non-Compliance: Even with the best evidence, patient adherence to recommended treatments can be a challenge.
Overcoming these barriers is crucial for the successful integration of evidence-based practice in nursing into routine care.
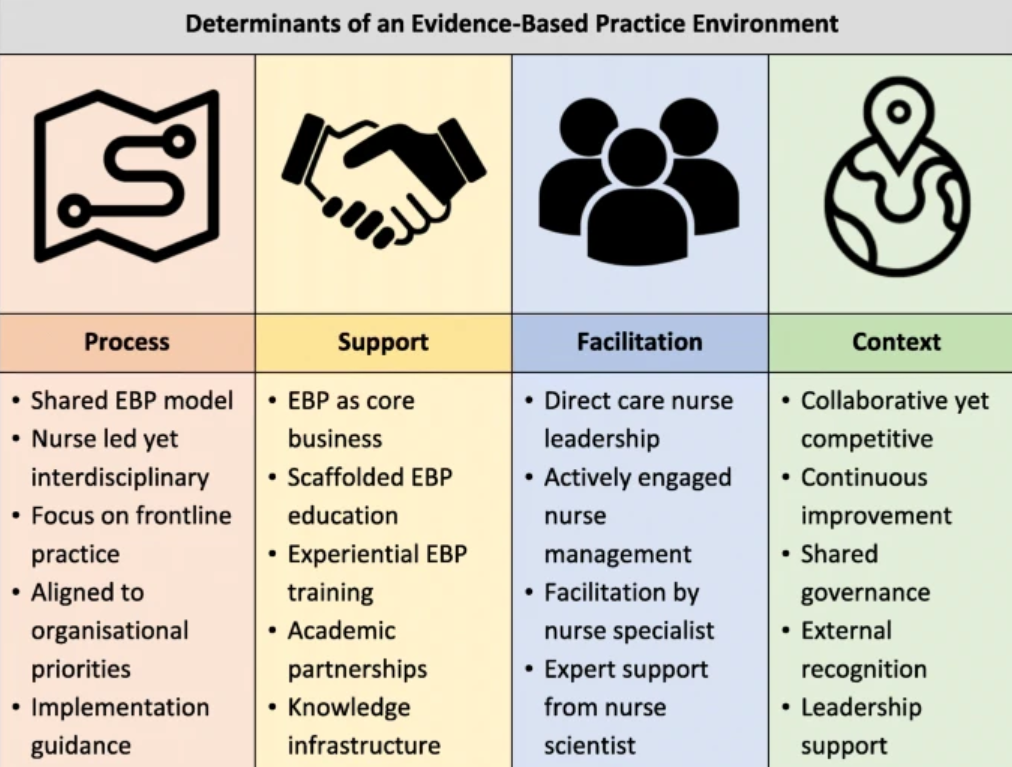
Strategies to Foster a Culture of Evidence-Based Practice in Nursing
Creating an environment where evidence-based practice in nursing thrives requires a multi-faceted approach involving individual nurses, managers, educators, and healthcare organizations:
- Leadership and Management Support:
- Allocate resources (time, funding, access to databases).
- Champion EBP initiatives and provide visible support.
- Integrate EBP into organizational policies, mission, and vision.
- Recognize and reward EBP efforts.
- Education and Training:
- Provide ongoing education on EBP principles and skills (PICO, searching, appraisal).
- Offer workshops, journal clubs, and mentorship programs.
- Integrate evidence-based practice in nursing competencies into nursing school curricula and new graduate orientation programs.
- Mentorship and Role Models:
- Identify EBP champions and mentors who can guide and support colleagues.
- Advanced Practice Registered Nurses (APRNs) and nurse researchers can play a key role.
- Dedicated Time for EBP:
- Incorporate EBP activities into job descriptions and work schedules.
- Protect time for nurses to engage in research and EBP projects.
- Access to Resources:
- Ensure easy access to computers, internet, and key research databases.
- Provide access to critical appraisal tools and EBP guidelines.
- Collaboration and Teamwork:
- Foster interdisciplinary collaboration on EBP projects.
- Create EBP committees or workgroups.
- Small-Scale Implementation:
- Start with small, manageable EBP projects to build confidence and demonstrate success.
- Focus on high-priority clinical problems.
- Dissemination of Findings:
- Share successful EBP initiatives within the organization and beyond (e.g., presentations, publications).
- Celebrating successes reinforces the value of evidence-based practice in nursing.
- Integrating EBP into Performance Appraisals:
- Recognize and reward staff who actively participate in evidence-based practice in nursing.
The Role of Individual Nurses in Advancing Evidence-Based Practice
Every nurse, regardless of their role or experience level, has a part to play in promoting and utilizing evidence-based practice in nursing:
- Cultivate a Spirit of Inquiry: Constantly question current practices. Ask “Why are we doing this?” and “Is there a better way?”
- Commit to Lifelong Learning: Stay updated with new research and clinical guidelines relevant to your practice area.
- Develop EBP Skills: Actively seek opportunities to learn about literature searching, critical appraisal, and research utilization.
- Participate in EBP Projects: Volunteer for EBP committees or offer to assist with EBP initiatives on your unit.
- Read and Discuss Research: Join a journal club or informally discuss research articles with colleagues.
- Collaborate with an Interdisciplinary Team: Work with physicians, pharmacists, therapists, and other healthcare professionals to implement evidence-based care.
- Advocate for Patients: Use evidence to support your clinical decisions and advocate for the best possible care for your patients.
- Be a Change Agent: Even small changes based on evidence can make a difference. Be willing to challenge outdated practices respectfully and constructively. The continuous improvement cycle is central to evidence-based practice in nursing.
EBP Nursing: Bridging Research and Practice
The term “EBP nursing” emphasizes the specific application of these principles within the nursing profession. It highlights the unique role nurses play in identifying clinical problems, finding and appraising evidence from a nursing perspective, and implementing changes that directly impact patient care delivered by nurses. Evidence-based practice in nursing is not about blindly following research; it’s about thoughtfully integrating it.
For students or nurses undertaking academic work, topics like “help with a paper about evidence-based practice in nursing” or “nursing research paper writing” become highly relevant. These academic exercises are designed to build the foundational skills necessary for lifelong engagement with evidence-based practice in nursing. Understanding research methodology, learning how to critique studies, and synthesizing information are all vital components.
In case you need help with choosing a topic, writing a research paper, case study, essay or dissertation about evidence-based practice in nursing, do not hesitate to engage PhD Nurse Writer. We offer a comprehensive service that covers topic suggestion, paper writing, proofreading, editing, formatting and plagiarism removal. Our writers can also offer customized help with assignments, term papers, TEAS tests and online classes.
The Future of Evidence-Based Practice in Nursing
The landscape of evidence-based practice in nursing is continually evolving, driven by technological advancements and a growing emphasis on personalized care:
- Big Data and Analytics: The ability to analyze large datasets from electronic health records (EHRs) will provide new insights and evidence to inform practice.
- Artificial Intelligence (AI): AI tools may assist in rapidly synthesizing evidence, identifying patterns, and supporting clinical decision-making.
- Increased Patient Involvement: Greater emphasis will be placed on shared decision-making and incorporating patient-reported outcomes into the evidence base.
- Implementation Science: More research will focus on how to effectively implement evidence-based interventions into diverse clinical settings, bridging the “know-do” gap that often hinders evidence-based practice in nursing.
- Global Collaboration: Increased sharing of research and best practices across international borders will enrich the body of evidence available for evidence-based practice in nursing.
Conclusion: Embracing Evidence-Based Practice in Nursing
Evidence-based practice in nursing is more than just a buzzword; it is a fundamental shift in how nurses approach patient care. It represents a commitment to excellence, continuous improvement, and the provision of care that is not only compassionate but also scientifically sound. By integrating the best research evidence with clinical expertise and patient values, nurses can significantly improve patient outcomes, enhance patient safety, and elevate the professional standing of nursing.
The journey towards fully embedding evidence-based practice in nursing into every aspect of care requires dedication, resources, and a cultural shift. However, the benefits for patients, nurses, and the healthcare system are undeniable. As the healthcare environment becomes increasingly complex, the principles of evidence-based practice in nursing will serve as an indispensable guide, ensuring that nurses remain at the forefront of delivering high-quality, effective, and patient-centered care.
Every nurse has a role to play in championing and implementing evidence-based practice in nursing, making it the standard, not the exception. The ongoing pursuit of knowledge and its application through evidence-based practice in nursing is what defines a truly professional nurse.