Table of Contents
The landscape of healthcare is undergoing a monumental transformation, driven largely by the rapid advancements in digital tools and communication platforms. At the heart of this evolution lies telehealth and technology integration, a dynamic duo reshaping how care is delivered, experienced, and managed. For nursing students on the cusp of entering this modernized profession, understanding and embracing telehealth and technology integration is no longer optional—it’s fundamental.
This guide provides a comprehensive overview, equipping future nurses with the knowledge and insights needed to navigate and excel in a healthcare environment increasingly reliant on telehealth and technology integration.
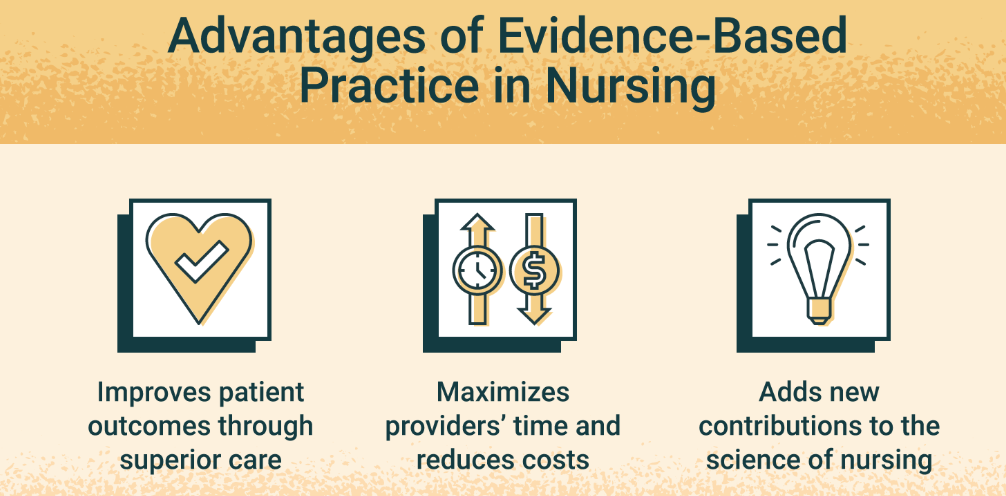
The very definition of patient care is expanding beyond the traditional confines of hospitals and clinics. Telehealth and technology integration allows for remote consultations, continuous monitoring, personalized patient education, and streamlined administrative processes. This paradigm shift promises enhanced access to care, improved patient outcomes, greater efficiency for providers, and a more patient-centered approach. As nursing students, your curriculum and clinical experiences will increasingly reflect the importance of telehealth and technology integration, preparing you for a career where digital literacy is as crucial as clinical skill.
What is Telehealth and Technology Integration?
To fully grasp the implications for your nursing career, let’s break down these interconnected terms.
- Telehealth: Broadly defined, telehealth encompasses the use of electronic information and telecommunications technologies to support and promote long-distance clinical health care, patient and professional health-related education, public health, and health administration. It’s not a single technology but a collection of methods.
- Synchronous Telehealth: Real-time interaction between a patient and provider (e.g., live video consultations, phone calls).
- Asynchronous Telehealth: “Store-and-forward” technology where patient data (images, medical history, lab results) is collected and sent to a specialist for review at a later time (e.g., dermatology, radiology).
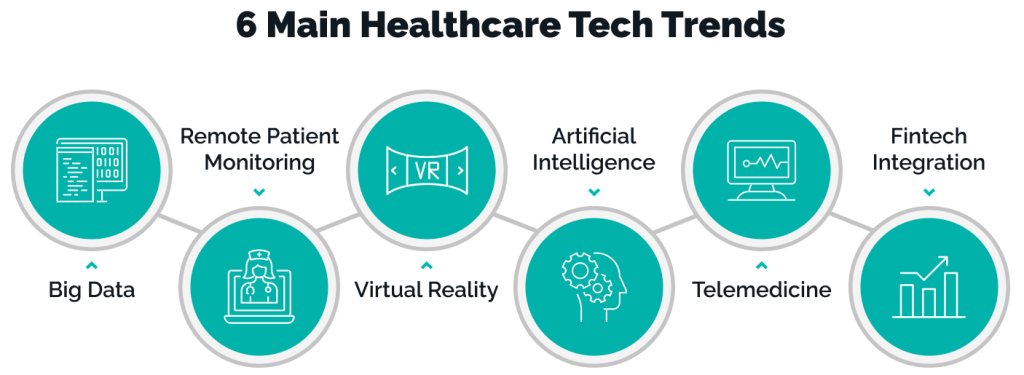
- Remote Patient Monitoring (RPM): Using digital technologies to collect medical and other forms of health data from individuals in one location and electronically transmit that information securely to health care providers in a different location for assessment and recommendations.
- Mobile Health (mHealth): Healthcare and public health practice and information supported by mobile devices such as smartphones, tablets, and wearable sensors.
- Technology Integration: This refers to the strategic incorporation of various technologies into the workflows and processes of healthcare delivery. It’s about more than just having new gadgets; it’s about making these tools work seamlessly together to improve care. This includes:
- Electronic Health Records (EHRs) / Electronic Medical Records (EMRs)
- Clinical decision support systems
- Patient portals
- Secure messaging platforms
- Data analytics and artificial intelligence (AI)
- Wearable devices and Internet of Things (IoT) in healthcare

The synergy between these two is where the true power lies. Effective telehealth and technology integration means that telehealth services are not standalone offerings but are deeply embedded within the broader technological infrastructure of a healthcare system, sharing data, streamlining communication, and enhancing the overall care continuum. This robust telehealth and technology integration is key to realizing its full potential.
The Role of Nurses in Telehealth and Technology Integration
Nurses are often the frontline users and facilitators of telehealth and technology integration. Your role will be multifaceted and critical to its successful implementation and adoption.
- Virtual Patient Assessment and Triage:
- Conducting comprehensive health assessments via video or phone.
- Utilizing digital stethoscopes, otoscopes, and other peripherals.
- Making critical decisions about the level of care needed based on remote interactions.
- Patient Education and Support:
- Educating patients on managing chronic conditions using telehealth tools.
- Guiding patients on how to use RPM devices or mHealth apps.
- Providing emotional support and health coaching remotely.
- Ensuring patients understand the nuances of telehealth and technology integration for their care.
- Remote Monitoring and Management:
- Reviewing data from RPM devices (e.g., blood pressure, glucose levels, weight, oxygen saturation).
- Identifying trends or alerts that require intervention.
- Collaborating with physicians and other team members based on monitored data.
- Care Coordination:
- Facilitating communication between patients, specialists, and primary care providers.
- Scheduling follow-up virtual or in-person appointments.
- Ensuring seamless transitions of care, supported by integrated technology.
- Advocacy and Quality Improvement:
- Advocating for patient access to telehealth services.
- Identifying challenges and opportunities for improving telehealth and technology integration workflows.
- Participating in research and quality improvement initiatives related to digital health. The field of telehealth and technology integration is constantly evolving, requiring continuous learning.
- Technical Support and Troubleshooting:
- Assisting patients with basic technical issues related to telehealth platforms or devices.
- Being the first point of contact when the telehealth and technology integration system presents a challenge for the patient.
sometimes, the specific roles of nurses in telehealth and technology integration might change, depending on the healthcare setting, patient needs and other factors. however, the roles defined above remain at the heart of nursing education and practice.
Essential Skills for Nursing Students in the Age of Telehealth
To thrive in this technologically advanced environment, nursing students must cultivate a specific set of skills beyond traditional clinical competencies.
- Digital Literacy and Technical Proficiency:
- Comfort with various software platforms (EHRs, telehealth portals, video conferencing).
- Ability to quickly learn and adapt to new technologies.
- Basic troubleshooting skills for common technical glitches. A solid foundation in telehealth and technology integration principles is vital.
- Enhanced Communication Skills:
- Virtual “Webside” Manner: Conveying empathy, active listening, and building rapport without physical presence.
- Clear and concise verbal and written communication.
- Ability to interpret non-verbal cues through a screen (or their absence).
- Explaining complex medical information and technology use in simple terms.
- Critical Thinking and Clinical Judgment:
- Making sound clinical decisions with potentially limited sensory input.
- Recognizing subtle cues that may indicate a patient’s condition is worsening.
- Knowing when a virtual visit is insufficient and an in-person assessment is required. The critical thinking applied to telehealth and technology integration ensures patient safety.
- Adaptability and Flexibility:
- The field of telehealth and technology integration is rapidly changing; nurses must be lifelong learners.
- Being open to new workflows and care delivery models.
- Managing unexpected technical issues or changes in patient presentation calmly.
- Ethical and Legal Acumen:
- Understanding HIPAA, HITECH, and state-specific regulations regarding telehealth, privacy, and data security.
- Ensuring patient consent and maintaining confidentiality in a digital environment.
- Navigating licensure issues, especially when providing care across state lines. A deep understanding of the ethical implications of telehealth and technology integration is crucial.
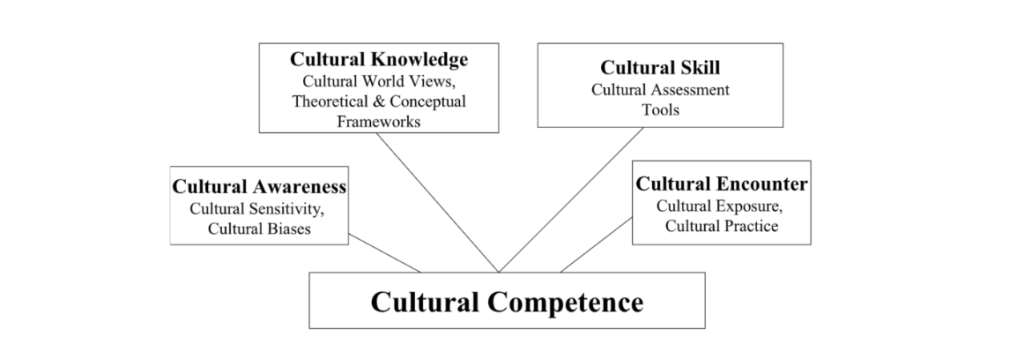
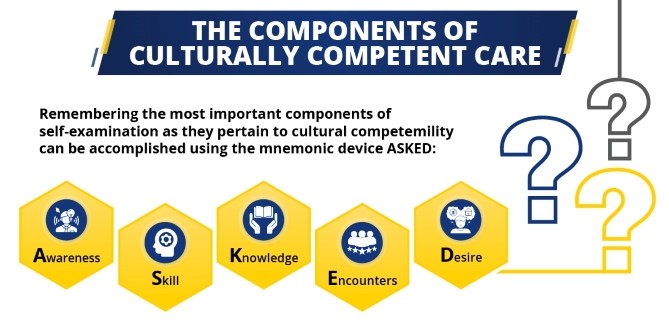
- Cultural Competency:
- Recognizing how cultural factors can influence a patient’s comfort with and access to technology.
- Adapting communication styles to diverse patient populations in a virtual setting.

Navigating the Challenges and Considerations
While telehealth and technology integration offers immense benefits, it’s not without its challenges. Nursing students should be aware of these to become effective problem-solvers and advocates.
- The Digital Divide:
- Access: Not all patients have reliable internet access, smartphones, or computers.
- Literacy: Some patients may lack the technical skills to use telehealth platforms.
- Equity: This can exacerbate existing health disparities if not addressed proactively. Strategies for equitable telehealth and technology integration are essential.
- Data Security and Privacy:
- Protecting sensitive patient health information (PHI) transmitted and stored digitally is paramount.
- Risk of data breaches and cyberattacks.
- Ensuring compliance with all privacy regulations is a cornerstone of safe telehealth and technology integration.
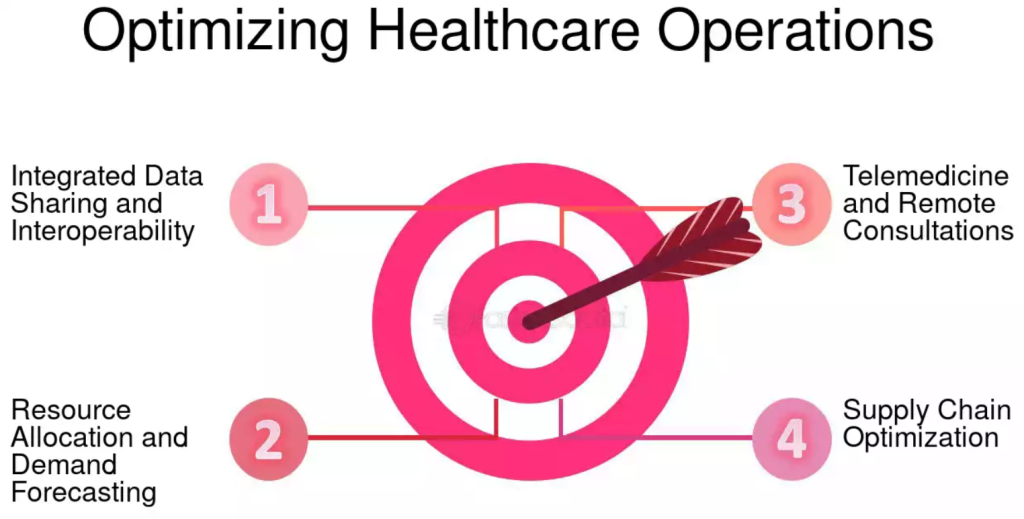
- Interoperability:
- The ability of different information systems, devices, and applications to access, exchange, integrate, and cooperatively use data in a coordinated manner.
- Lack of interoperability can create data silos and hinder seamless telehealth and technology integration.
- Reimbursement and Regulation:
- Payer policies for telehealth services can be complex and vary.
- Evolving state and federal regulations require ongoing attention.
- Workflow Integration and Resistance to Change:
- Integrating telehealth seamlessly into existing clinical workflows can be challenging.
- Overcoming resistance to change from both providers and patients. Effective change management is key for successful telehealth and technology integration.
- Impersonal Care Concerns:
- Some patients and providers may feel that telehealth lacks the personal touch of in-person visits.
- Nurses play a key role in humanizing virtual care experiences through strong communication and empathy.
Preparing for Your Future: How Nursing Education is Adapting
Nursing schools are increasingly recognizing the imperative to prepare students for a digitally-driven healthcare future. Look for programs and opportunities that emphasize telehealth and technology integration.
- Curriculum Enhancements:
- Dedicated courses or modules on telehealth, health informatics, and digital health technologies.
- Integration of telehealth and technology integration concepts across various nursing courses.
- Simulation and Skills Labs:
- Practicing virtual assessments using simulated patients and telehealth platforms.
- Hands-on experience with RPM devices and mHealth applications.
- Clinical Placements:
- Opportunities for clinical experiences in settings that utilize telehealth extensively (e.g., virtual urgent care, remote chronic disease management programs).
- Observing and participating in various forms of telehealth and technology integration.
- Interprofessional Education:
- Collaborating with students from other health professions (medicine, pharmacy, social work) on telehealth-based case studies or projects.
- Continuing Education and Certifications:
- Even after graduation, commit to ongoing learning in telehealth and technology integration.
- Consider certifications in health informatics or telehealth to enhance your expertise.
Research in Telehealth and Technology Integration: Advancing the Frontier
The field of telehealth and technology integration is a fertile ground for research. As nursing students, and later as practicing nurses, you may have opportunities to contribute to this growing body of knowledge.
- Areas for Investigation:
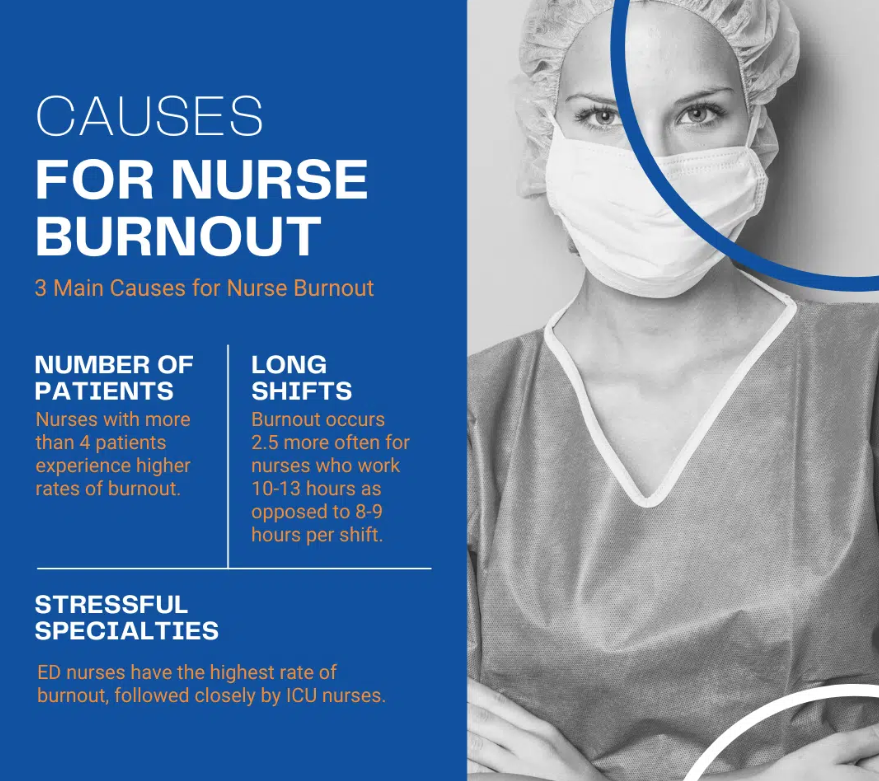
- Effectiveness of different telehealth modalities for various patient populations and conditions.
- Impact of telehealth and technology integration on patient outcomes, satisfaction, and access to care.
- Best practices for virtual nursing assessments and communication.
- Strategies to overcome the digital divide and ensure equitable access.
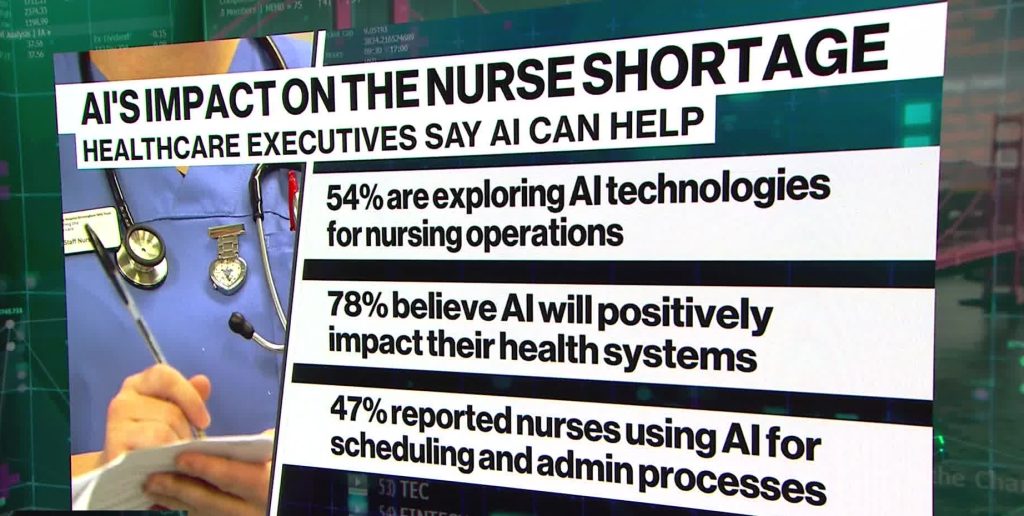
- The role of AI and machine learning in enhancing telehealth.
- Ethical considerations in the use of advanced telehealth and technology integration.
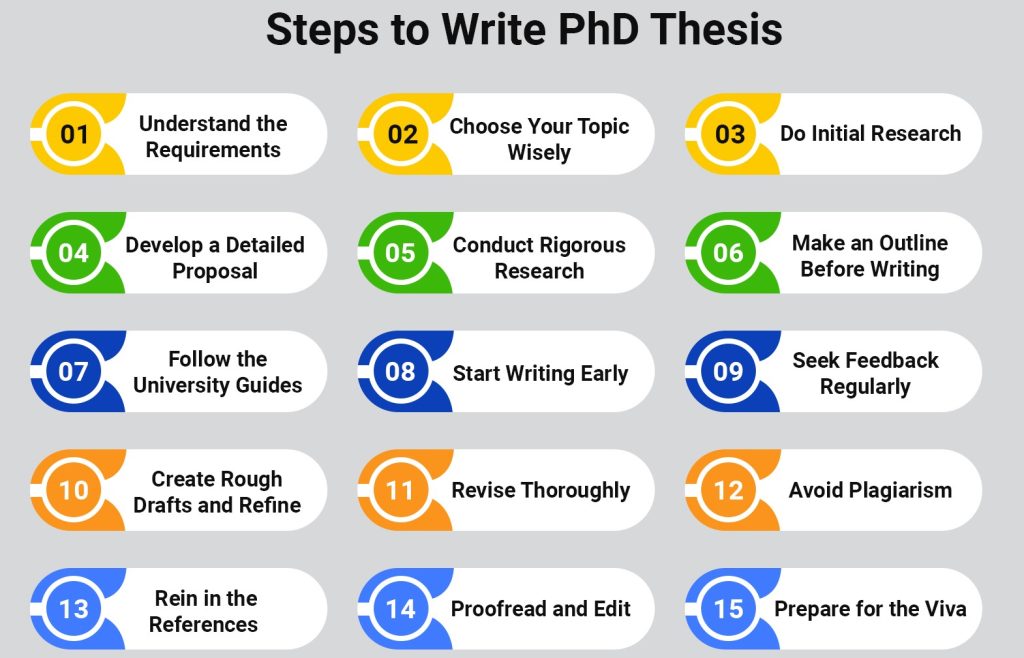
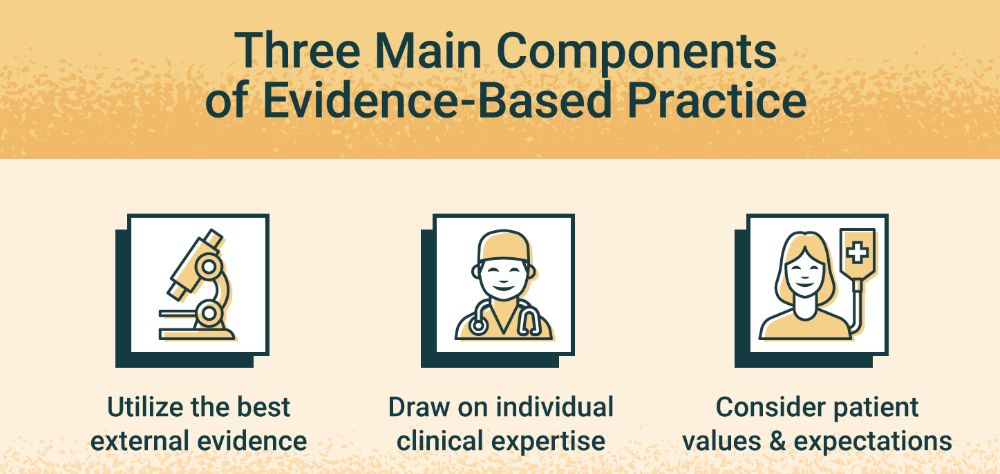
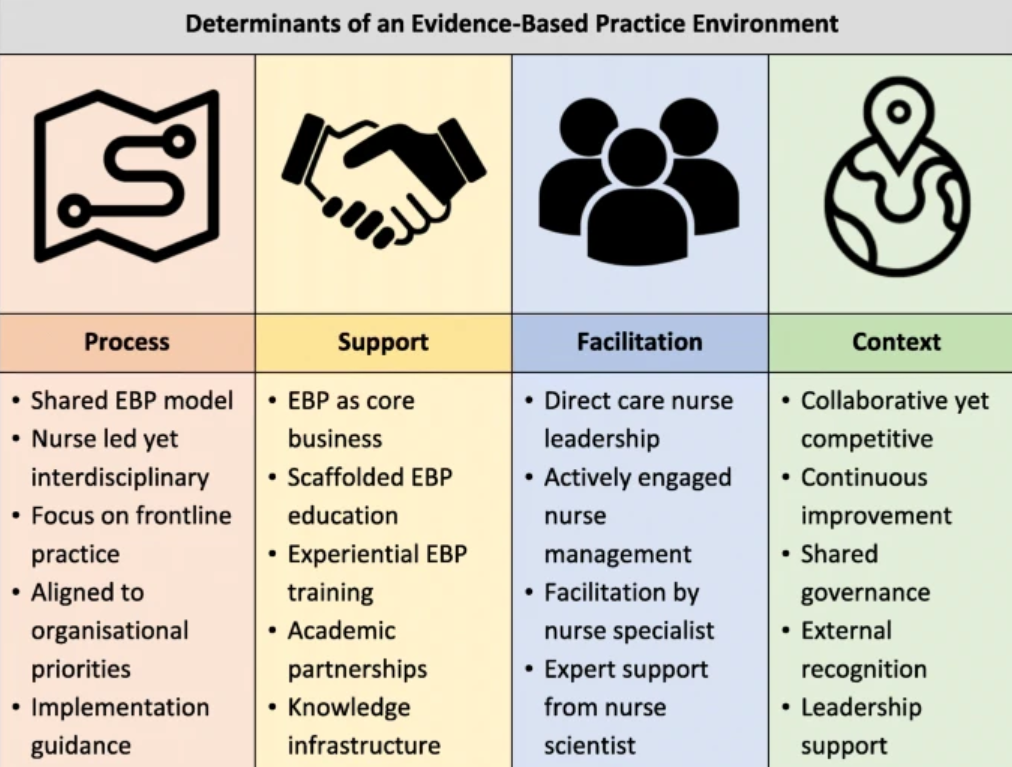
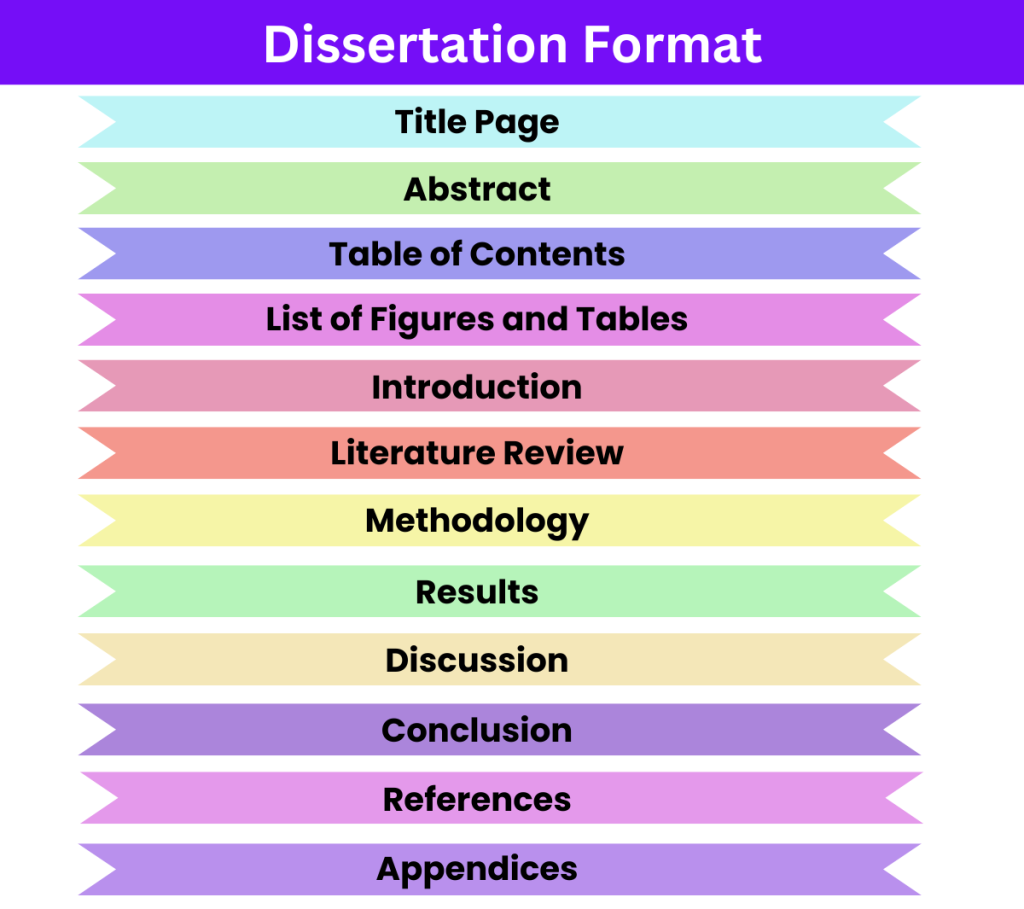
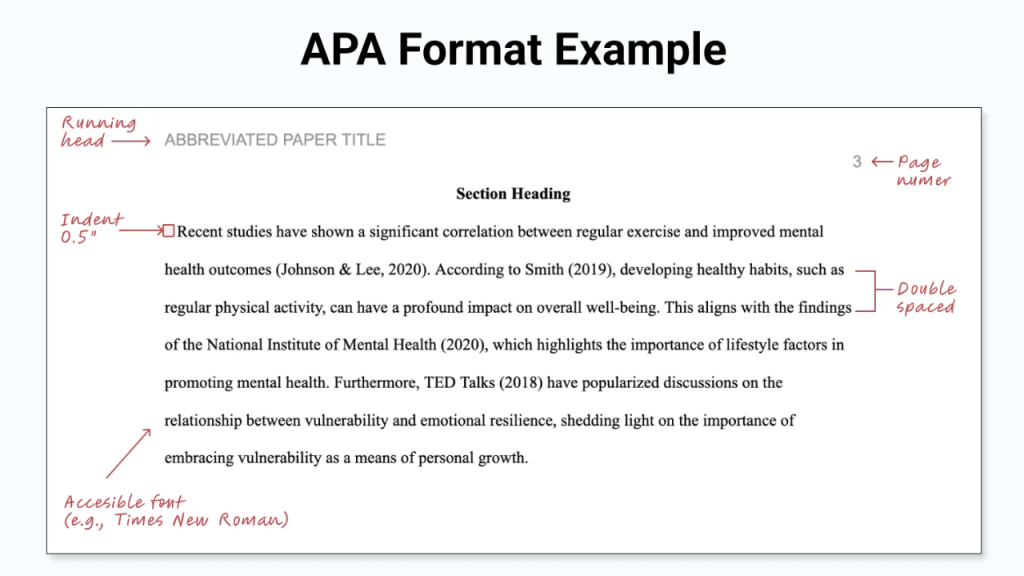
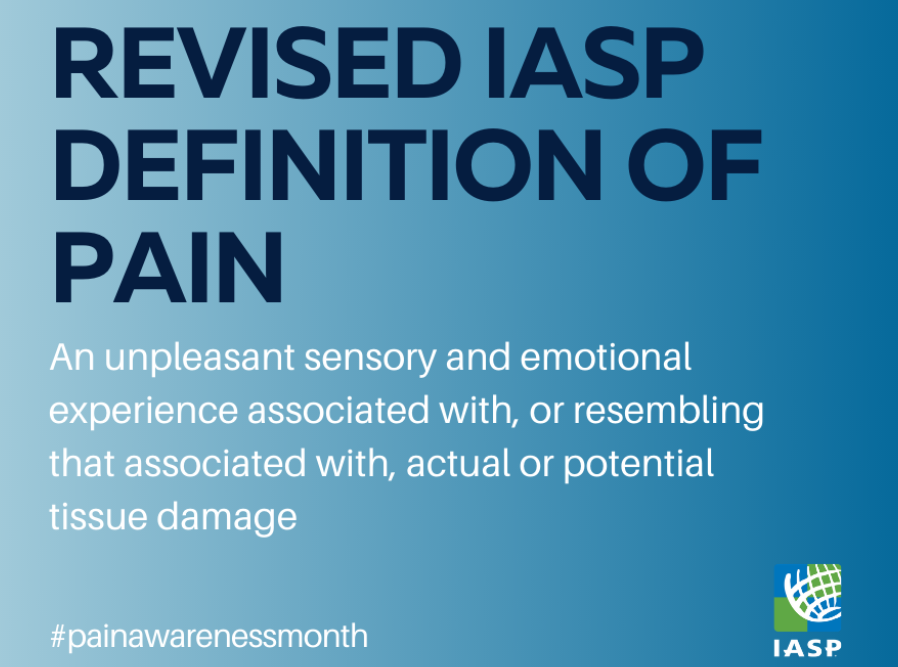
For those pursuing advanced degrees, opportunities to help with telehealth and technology integration research are plentiful. You might find yourself contributing to a groundbreaking study, or even undertaking your own research paper about telehealth and technology integration. For doctoral candidates, a telehealth and technology integration dissertation could explore complex issues, contributing significantly to evidence-based practice (EBP) in this domain.
At PhD Nurse Writer, we help students with writing authentic and impactful nursing research papers and dissertations. We can assist you with topic suggestion, paper writing, proofreading, editing, formatting and plagiarism removal. Our experts can also help with assignments, term paper writing, proctored exams, essays and case studies for academic excellence. we guarantee a personalized service that will truly give you peace of mind while also ensuring the best grades in all your exams.
The evidence generated through such research is vital for refining and optimizing telehealth and technology integration strategies worldwide. Continuous research ensures that telehealth and technology integration evolves to meet the changing needs of patients and providers.
Powerful Telehealth and Technology Integration Topic Ideas
At the heart of the global healthcare transformation lies the powerful synergy of telehealth and technology integration. This isn’t just about video calls with doctors; it’s about creating a seamless, intelligent, and patient-centric healthcare ecosystem. Exploring innovative ideas in this domain is crucial for shaping a healthier future.
Below are some potent topic ideas ripe for exploration and development in the realm of telehealth and technology integration. These topics ideas are ideal for nursing essays, research papers, dissertations and even case studies.
1. The AI-Powered Personalized Patient Journey
Artificial Intelligence (AI) is no longer a futuristic concept but a present-day tool with immense potential in healthcare. Integrating AI deeply into telehealth platforms can revolutionize patient care.
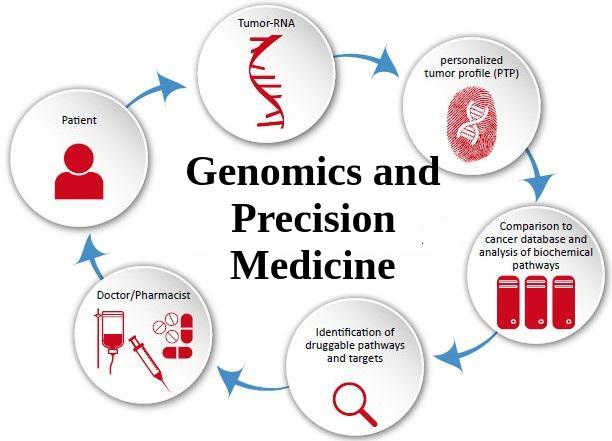
- Predictive Analytics for Proactive Care: AI algorithms can analyze patient data (from wearables, EHRs, and telehealth interactions) to predict potential health risks, allowing for early interventions and personalized preventative care plans delivered via telehealth.
- AI-Driven Diagnostic Support: AI can assist clinicians during telehealth consultations by analyzing symptoms, medical history, and even visual cues (with patient consent) to suggest potential diagnoses or necessary tests, improving accuracy and efficiency.
- Intelligent Virtual Assistants & Chatbots: AI-powered chatbots can handle initial patient queries, schedule appointments, provide medication reminders, and offer basic health information, freeing up human staff for more complex cases. This is a core component of effective telehealth and technology integration.
2. Immersive Technologies: VR/AR in Remote Healing and Training
Virtual Reality (VR) and Augmented Reality (AR) offer novel ways to enhance the telehealth experience, moving beyond simple video interactions.
- VR for Remote Physical Therapy and Pain Management: Patients can engage in guided physical therapy sessions in immersive virtual environments from their homes, with therapists monitoring progress remotely. VR can also be used for pain distraction and management techniques.
- AR-Enhanced Surgical Consultations and Training: Surgeons could use AR to overlay medical imaging onto a patient’s view during a telehealth consultation or even guide local practitioners in remote procedures. It also offers powerful tools for remote medical training.
- Mental Health Therapy through VR: Creating safe, controlled virtual environments for exposure therapy, mindfulness exercises, or social skills training can significantly benefit patients receiving mental healthcare via telehealth.

3. Seamless Wearable and IoT Integration for Continuous Care
The Internet of Things (IoT) and wearable devices generate a constant stream of health data. The true power comes when this data is intelligently integrated into telehealth systems.
- Real-Time Remote Patient Monitoring (RPM): Advanced wearables can track vital signs, sleep patterns, activity levels, and specific biomarkers. Integrating this data directly into telehealth platforms allows for continuous monitoring of chronic conditions and early alerts for clinicians.
- Automated Data-Driven Interventions: Based on RPM data, telehealth systems could trigger automated responses, such as medication reminders, educational content, or even alerts to caregivers or emergency services. This proactive telehealth and technology integration can be life-saving.
- Personalized Lifestyle Recommendations: By analyzing long-term data from wearables, telehealth platforms can offer highly personalized advice on diet, exercise, and lifestyle adjustments to improve overall health outcomes.
The journey towards a fully optimized healthcare system is paved with innovative telehealth and technology integration. These ideas represent just the tip of the iceberg. As technology continues to evolve, so too will the opportunities to create more accessible, efficient, and personalized healthcare experiences for everyone. The future relies on our continued exploration and implementation of these powerful telehealth and technology integration strategies.
Embracing Telehealth and Technology Integration
The integration of telehealth into routine healthcare is not a futuristic concept; it’s the current reality and the clear path forward. The COVID-19 pandemic accelerated this adoption, but the underlying drivers—the need for greater access, efficiency, and patient-centeredness—ensure that telehealth and technology integration will continue to expand and evolve.
As a nursing student, your journey into this dynamic field is beginning at an exciting time. By proactively seeking knowledge, developing essential digital and communication skills, and maintaining a patient-centered focus, you will be well-prepared to leverage the power of telehealth and technology integration to provide exceptional care. Your ability to adapt and innovate within this realm will define your success and your contribution to the future of nursing.
Embrace the learning curve, engage with the technology, and remember that at the heart of all telehealth and technology integration efforts is the commitment to improving human health and well-being. The future of nursing is intrinsically linked with telehealth and technology integration, and you are poised to be at the forefront of this transformation. This comprehensive approach to telehealth and technology integration will serve you well throughout your career. The ongoing development of telehealth and technology integration promises even more exciting possibilities for patient care.