
Table of Contents
Nursing is a complex and dynamic profession that demands a comprehensive understanding of patient needs. The foundation of effective nursing practice lies in the meticulous process of patient assessment, which involves gathering data, analyzing findings, and formulating a plan of care.
This article delves into a real-world nursing case study on patient assessment, highlighting the importance of this crucial step in providing holistic and patient-centered care.
What is Patient Assessment?
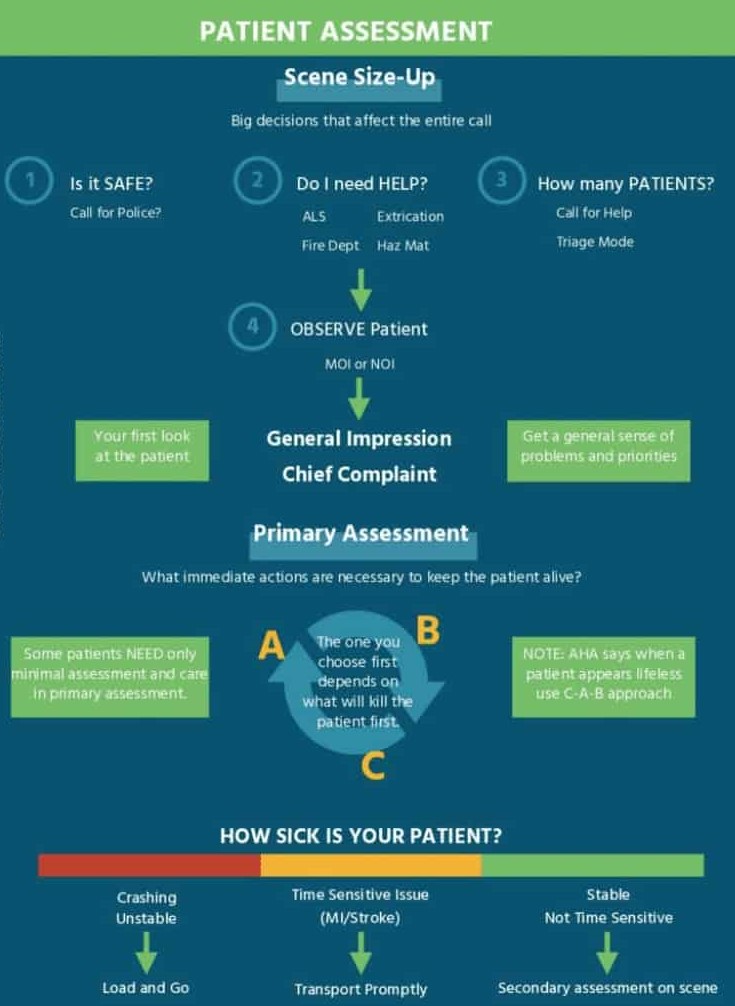
Patient assessment is the systematic process of gathering and analyzing information about a patient’s health status. It involves collecting data, interpreting findings, and formulating a plan of care. This crucial step in the nursing process helps nurses understand the patient’s needs and develop the most appropriate interventions.
Elements of Patient Assessment:
- Health History: Gathering information about the patient’s medical history, family history, social history, and current health concerns.
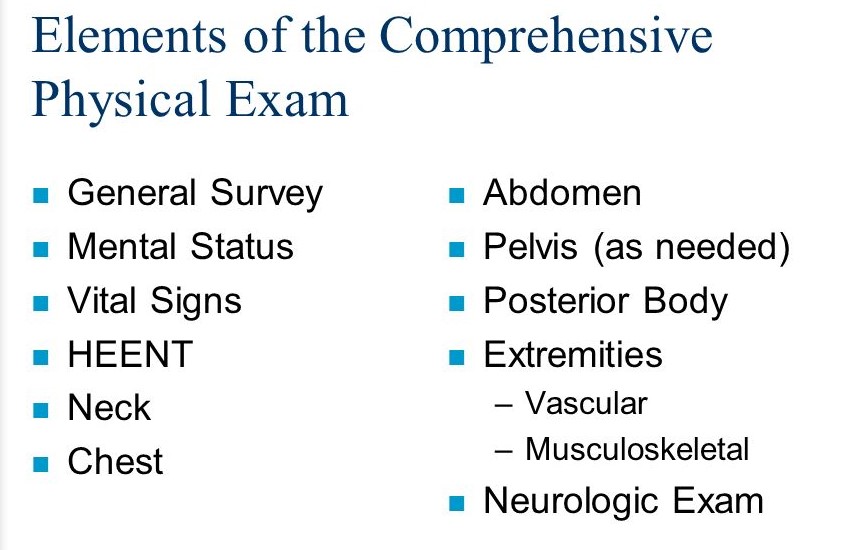
- Physical Assessment: Observing the patient’s physical appearance, vital signs, and conducting a thorough head-to-toe examination.
- Psychological Assessment: Evaluating the patient’s emotional state, coping mechanisms, and mental status.
- Social Assessment: Understanding the patient’s support system, social determinants of health, and environmental factors that may influence their well-being.
Purpose of Patient Assessment:
- Identify Health Problems: Determine the patient’s current health status and identify any potential problems.
- Develop a Care Plan: Formulate a personalized care plan based on the patient’s individual needs.
- Evaluate Progress: Monitor the patient’s progress throughout their care and make adjustments as needed.
- Promote Patient Safety: Identify potential risks and implement preventive measures to ensure patient safety.
Nursing Case Study on Patient Assessment: This crucial process forms the basis for all nursing care.
Nursing Case Study on Patient Assessment: A thorough assessment helps identify the patient’s individual needs and guide the nursing interventions.
Nursing Case Study on Patient Assessment: Through careful analysis of the assessment data, nurses can develop a comprehensive and personalized care plan.
Patient assessment is a fundamental aspect of nursing practice. It is a dynamic and ongoing process that helps nurses provide safe, effective, and compassionate care. By utilizing a variety of assessment tools and techniques, nurses can gain a comprehensive understanding of their patients’ needs and deliver individualized care that promotes optimal health outcomes.
Tips for Crafting a Compelling Nursing Case Study on Patient Assessment
1. Start with a Strong Introduction:
- Grab the reader’s attention: Begin with a concise and engaging overview of the patient’s presenting problem and why this nursing case study on patient assessment is relevant.
- Clearly state the purpose: Explain why you’re writing this case study, such as to demonstrate the importance of a comprehensive assessment, highlight a specific nursing skill, or analyze a challenging patient situation.
2. Provide a Detailed and Organized Account:
- Comprehensive data collection: Capture all relevant information gathered during the nursing case study on patient assessment, including vital signs, medical history, medication list, social history, family history, and psychosocial factors.
- Organized presentation: Structure your case study logically. Use headings and subheadings to organize the assessment data into categories like physical exam findings, subjective reports, and diagnostic tests.
3. Analyze and Interpret the Data:
- Go beyond just listing findings: Don’t simply present the assessment data; analyze it to identify patterns, draw conclusions, and link findings to potential diagnoses or nursing diagnoses.
- Explain the reasoning behind your actions: Clearly demonstrate how the nursing case study on patient assessment informed your decisions regarding patient care, treatment recommendations, and interventions.

4. Reflect on the Case and Its Implications:
- Consider the broader context: How does this nursing case study on patient assessment relate to the overall patient experience, their healthcare needs, and the nursing process?
- Discuss the ethical and legal considerations: If relevant, address any ethical or legal dilemmas encountered during the nursing case study on patient assessment and how you addressed them.
5. Ensure Clear and Concise Writing:
- Maintain a professional tone: Use clear, concise language that is appropriate for a healthcare audience. Avoid jargon and unnecessary technical terms.
- Be objective: Present the facts objectively without personal opinions or biases. Focus on the data and your rationale for the actions taken.
By following these tips, you can write a compelling nursing case study on patient assessment that demonstrates your understanding of the assessment process, your critical thinking skills, and your ability to provide safe and effective nursing care.
Sample Nursing Case Study on Patient Assessment
Sample Case Study: Mrs. Johnson, a 72-year-old with a History of Heart Failure
Mrs. Johnson, a 72-year-old widow, presents to the emergency department (ED) with shortness of breath, fatigue, and lower extremity edema. She has a history of congestive heart failure (CHF) and has been experiencing worsening symptoms over the past week. This nursing case study on patient assessment will focus on the steps taken by the nurse to thoroughly assess Mrs. Johnson and develop a personalized plan of care.
The Assessment Process: A Multi-Dimensional Approach
The nursing case study on patient assessment begins with the initial encounter, where the nurse performs a comprehensive assessment encompassing physical, emotional, and social aspects of Mrs. Johnson’s health.
1. Initial Assessment: Gathering Vital Clues
- Vital Signs: The nurse immediately assesses Mrs. Johnson’s vital signs, which reveal an elevated heart rate (110 beats per minute), rapid respiratory rate (24 breaths per minute), low oxygen saturation (88%), and elevated blood pressure (160/90 mmHg). These findings suggest a potential exacerbation of her CHF.
- History of Present Illness (HPI): A detailed HPI elicits information about the onset, duration, and characteristics of her symptoms. Mrs. Johnson reports her shortness of breath started gradually over the past week and has been worsening, particularly with exertion. She also describes fatigue, difficulty sleeping, and swelling in her ankles and feet.
- Past Medical History (PMH): The nurse carefully reviews Mrs. Johnson’s PMH, noting her history of CHF, hypertension, and type 2 diabetes. This information provides valuable insights into her current condition and potential risk factors.
- Medications: The nurse inquires about her current medications, including their dosages and frequency. Mrs. Johnson reports taking diuretics, ACE inhibitors, beta-blockers, and insulin for her diabetes. This information is critical for assessing potential drug interactions and adjusting her medication regimen as needed.
- Allergies: The nurse carefully records any allergies, including food, medication, and environmental allergies. This information ensures safety during the provision of care.
2. Physical Examination: Unveiling the Body’s Story
The physical examination in this nursing case study on patient assessment involves a head-to-toe assessment to identify any physical signs that may indicate the severity of her condition.
- Respiratory System: Auscultation of the lungs reveals crackles in both lung bases, suggesting fluid buildup in the lungs. This observation confirms the suspicion of pulmonary edema, a common complication of CHF.
- Cardiovascular System: Examination of the heart reveals an irregular rhythm with a gallop, indicating an abnormal heart rate and rhythm.
- Peripheral Vascular System: Palpation of the peripheral pulses reveals weak pulses in the lower extremities, indicative of decreased blood flow.
- Gastrointestinal System: Inspection of the abdomen reveals distention and tenderness, suggesting fluid accumulation in the peritoneal cavity (ascites).
- Skin: The nurse observes edema in the lower extremities, particularly around the ankles and feet. This finding supports the diagnosis of fluid overload, which is a hallmark of CHF exacerbation.
3. Psychosocial Assessment: Understanding the Whole Person
This nursing case study on patient assessment extends beyond the physical realm to encompass Mrs. Johnson’s emotional and social well-being.
- Emotional Status: The nurse observes that Mrs. Johnson appears anxious and worried about her condition. She expresses concern about her ability to manage her symptoms and perform her daily activities.
- Social Support: The nurse inquires about her living situation and support system. Mrs. Johnson lives alone and has limited support from family and friends. She reports feeling overwhelmed and isolated, highlighting the importance of addressing her social needs.
4. Pain Assessment: Addressing Suffering
The nurse assesses Mrs. Johnson’s pain levels using a pain scale, noting any associated symptoms. She reports experiencing mild discomfort in her chest and legs, which she describes as a “tightness” sensation. This finding suggests potential cardiac ischemia, another complication of CHF.
5. Laboratory and Diagnostic Tests:
The nurse collaborates with the medical team to order appropriate laboratory and diagnostic tests to further evaluate Mrs. Johnson’s condition.
- Electrocardiogram (ECG): An ECG confirms the presence of an abnormal heart rhythm, indicating the need for further cardiovascular evaluation.
- Chest X-ray: A chest x-ray reveals fluid buildup in the lungs, confirming the presence of pulmonary edema.
- Blood Work: Blood tests, including complete blood count (CBC), electrolyte panel, and cardiac enzymes, provide information about Mrs. Johnson’s overall health and potential organ function impairment.
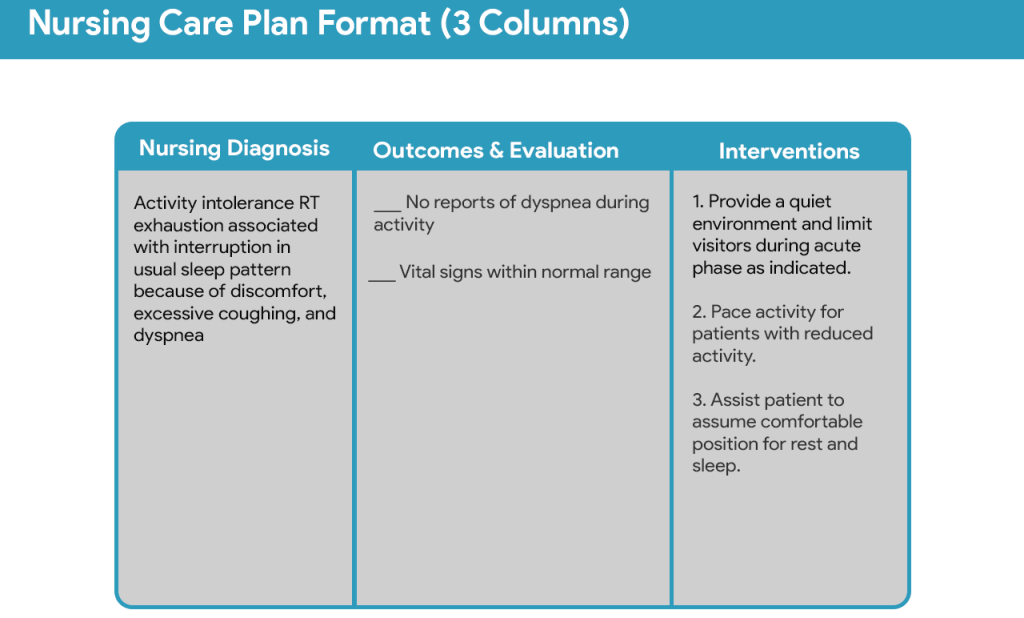
Nursing Diagnosis and Plan of Care
Based on the nursing case study on patient assessment, the nurse develops a comprehensive plan of care that addresses the identified health issues. The key nursing diagnoses for Mrs. Johnson include:
- Ineffective Breathing Pattern Related to Pulmonary Edema
- Excess Fluid Volume Related to Impaired Cardiac Function
- Activity Intolerance Related to Fatigue and Dyspnea
- Anxiety Related to Illness and Hospitalization
- Risk for Social Isolation Related to Limited Social Support
The nursing plan of care focuses on:
- Improving Respiratory Function: Administration of oxygen therapy, elevating the head of the bed, and monitoring respiratory status are crucial to alleviate dyspnea and improve oxygenation.
- Managing Fluid Overload: The nurse administers diuretics as prescribed to remove excess fluid from the body. Careful monitoring of fluid intake and output is essential to ensure effective fluid management.
- Enhancing Activity Tolerance: The nurse encourages gradual activity and rest periods to prevent fatigue and conserve energy. Activities should be individualized based on Mrs. Johnson’s current level of tolerance.
- Reducing Anxiety: The nurse provides emotional support, explains procedures and treatments, and answers questions to alleviate anxiety and promote a sense of control.
- Promoting Social Interaction: The nurse connects Mrs. Johnson with social workers or other support services to address her social isolation and provide resources.
Evaluation and Follow-Up:
The nursing case study on patient assessment extends beyond the initial assessment and care plan. The nurse continuously evaluates Mrs. Johnson’s response to treatment, monitors her vital signs, and adjusts the plan of care as needed. This ongoing evaluation ensures the effectiveness of interventions and promotes her overall well-being.
Outcomes:
With timely and effective nursing interventions, Mrs. Johnson’s symptoms gradually improve. Her breathing becomes easier, her edema reduces, and her anxiety subsides. The nurse collaborates with the medical team to discharge Mrs. Johnson with appropriate home health services and medication management to ensure continuity of care.
Learning Points from This Nursing Case Study on Patient Assessment:
This nursing case study on patient assessment highlights several crucial learning points:
- Holistic Assessment: A comprehensive assessment that encompasses physical, emotional, and social aspects provides a complete picture of the patient’s needs and promotes holistic care.
- Data Collection and Analysis: Thorough data collection and analysis are critical for accurate diagnosis and development of an effective plan of care.
- Communication and Collaboration: Effective communication and collaboration between nurses and other healthcare professionals ensure coordinated care and improved patient outcomes.
- Patient-Centered Care: The nursing case study on patient assessment emphasizes the importance of patient-centered care by tailoring interventions to address individual needs and preferences.
- Continual Evaluation: Ongoing evaluation and adjustment of the plan of care based on the patient’s response ensure optimal outcomes and prevent complications.
Conclusion:
The nursing case study on patient assessment of Mrs. Johnson demonstrates the crucial role of nursing in providing personalized and effective care. Through a meticulous assessment process, nurses gather vital clues, interpret findings, and develop a comprehensive plan of care that addresses the patient’s physical, emotional, and social needs. This case study serves as a valuable reminder that patient assessment is the foundation of quality nursing practice and essential for delivering holistic, patient-centered care.
Key takeaways:
- Patient assessment is the foundation of effective nursing care.
- A comprehensive assessment includes physical, emotional, and social components.
- Nurses play a crucial role in data collection, analysis, and interpretation.
- Communication and collaboration are essential for providing coordinated care.
- Patient-centered care prioritizes individual needs and preferences.
- Ongoing evaluation and adjustment of the plan of care are critical for optimal outcomes.
This nursing case study on patient assessment emphasizes the importance of this process in achieving quality care for all patients. By applying these principles, nurses can empower patients, enhance their well-being, and contribute to positive health outcomes.
Get Nursing Case Study Writing Help for Patient Assessment
Writing a stellar nursing case study on patient assessment can be daunting, especially to beginners. However, you can easily avoid the stress with a customized nursing case study from PhD Nurse Writer. We offer professional nursing case study writing help, with a guarantee of original and compelling papers. Our experienced writers can also assist you with nursing research papers, essays and dissertations.





